We had a question via Twitter last week regarding a left/right discrimination finding from Perth physio Jay Tan:
“@noigroup @altThinq What do you do when laterality assessment is worse on pain free side? What’s your interpretation? #gmi”
@JayS_Tan
I checked with Jay and he was happy for me to post this question on noijam so that we could discuss it in more than 140 characters.
Jay explained further that the client’s recognise results were slower on the unaffected side compared to norms as well as compared to the painful side.
Lets have a look at what some of the science says
Implicit motor imagery
The Graded Motor Imagery Handbook provides a detailed discussion of the science and understanding of what’s going on in the brain when a person performs an implicit left/right judgement.
You can get a taste of this here, with a series of free GMI Posters.
Here are some key points:
-Implicit motor imagery (left/right judgements)occurs when the person performing the judgement is not aware that they are mentally ‘moving’
-During implicit motor imagery, premotor cells modify primary motor cells without activating them
-Implicit motor imagery is less likely to activate a pain neurotag than explicit motor imagery (the person is aware that they are mentally moving) and mirror therapy.
– Data suggests that a left/right discrimination accuracy of about 80%, a response time of 2 seconds +/- .5 for hands and feet, 1.6 seconds +/- .5 for backs and necks, with equal results left and right, is normal.
Making sense of the results
The Graded Motor Imagery Handbook provides a model for understanding the results of performing an implicit left right judgement based on the most up to date research, trials and brain science.
The interpretation of the results of a left/right judgement test will vary dependent on whether the injury is acute or chronic (shaky territory with those “definitions” I know, but bear with me).
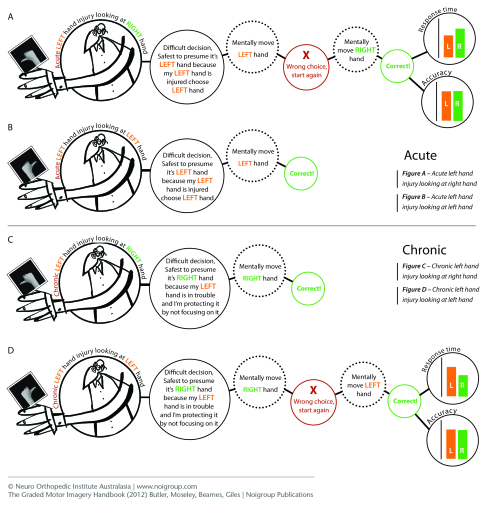
With an acute left hand injury, when faced with the difficult decision of quickly determining if a viewed image of a right hand is a left or a right hand, the safest presumption is that the image is a left hand because this is the injured hand. The left hand is mentally moved, outside of awareness, and an internal check reveals that this is incorrect. The process occurs over – choose right hand, mentally move right hand and check, and this time the result is correct and the process results in a response, that is selecting “right” via the method being used to test laterality.
When a person with an acute left hand injury is faced with deciding whether a viewed image of a left hand is left or right, the same process occurs, but this time the initial presumption is correct.
The initial presumption towards the acutely injured left hand results in a faster response time for left images. That is, in an acute injury situation, the person is faster to recognise images of/relating to their injured side.
In a chronic pain state things are different, in fact, usually opposite. In a chronic pain state, the initial presumption is towards the non-painful side/part. The suggestion is that this is a protective response – it is safest for the person to presume that the image is of their non-painful part/side as they are protecting that part of themselves that is in trouble by not focussing on it.
This results in the person generally being slower to recognise images of/relating to their injured side.
The plot thickens
However, we know that clinically and anecdotally, there are some interesting and different presentations when people in trouble perform left/right judgements.
There’s an amazingly rich body of experience and knowledge out there from clinicians using Recognise™ Online or the Recognise™ apps providing great opportunity for ‘out of the shadows learning’.
Experiences outside of the norm challenge us to continue to think and question what might be happening in the brain of a person in trouble; to explore, to experiment and to use clinical reasoning powered up by modern neuroimmune science paradigms.
In answer to your question…
The explanation above might be enough to help answer Jay’s original question, however I want to open it to noijam readers – the superstar clinicians out there using Recognise™ and GMI every day, the noi faculty teaching the future superstar clinicians and anyone else interested in people with tricky pain states and how the brain responds and changes when faced with trouble- you’re all superstars too.
Questions, comments, thoughts and answers all welcome in the comments below.
– Tim Cocks
Tap into the most up to date Graded Motor Imagery Resources with a noigroup course or get your hands on the culmination of 15 years worth of neuroscience research and clinical trials in the Graded Motor Imagery Handbook with chapters covering all three stages of GMI, the science behind them, some pain education essentials and tips on progression and clinical reasoning.

I think the observation here is in identifying the “novelty”……. Maybe the brain has established that it believes the normal side to be abnormal? ……… Story of my life !!!!! ………I have often seen differences between left and right were it is the, so called normal side that is performing badly …….However, if we trust that what we observe is ” the truth” then we will always be capable of inventing a treatment fitting for the situation, and save the discussions of how, where, when and why for the staff room……..no ?????
Thanks Tim, David and Jay,
Jay asks “What do you do when laterality assessment is worse on the pain free side? What’s your interpretation?
We hear this occasionally at NOI amid the mass of clinical anecdote we receive and the first thing I do is marvel at the brain and reflect on how little we know about it!.
This feature is not common or it would probably have been picked up in some of the normative studies of the last few years. It may be syndrome specific and even within syndrome, ie there are many different “kinds” of CRPS. It is possibly related to the fact that researchers focus on the so called affected brain side, yet the so called and expected unaffected side may show change. I know there is some emerging research here that I will find and link to.
My suggestion is to accept it and continue on with the GMI process until we know any better.
David
Hi Jay
Great question. I have found similar changes in a number of people with persistent pain. This often includes a slowing of response times for non- or less-affected body parts/sides, whereby the affected body part being tested remains fairly normal. I have found this can also change depending on the bodily space that you are testing this in e.g. towards or away from the most affected body part. Some of this may relate to the relative attention given to that body part and ties in with data in some of the original trials ((Moseley et al 2005 Cog Brain Res 25: 188–194; Hudson et al 2006 Eur J Pain 10: 219-224). My question would be does this alter with repetition?
I have also found (not necessarily in isolation) that the accuracy may change more significantly in other body parts. This is difficult to understand but may relate to loss of precision of body representations and altered balance between hemispheres. It’s like they are putting huge effort in to keep the affected part normal at the detriment to the rest of the body i.e. not maintaining sufficient communication/processing of the unaffected body parts (cortically?) to maintain sufficient precision in bodily health.
I’d be interested to know how things go if you repeat the test in an unaffected body space or with the affected body part out of sight.
Thanks
Tim