“You and that bloody Explain Pain book. It made me completely rethink what I thought I knew, and question what I do as a clinician… your ears must’ve been burning at times with the things I said about you! I’ve read it twice and I think I’m starting to get it, BUT, where do I go now, what do I actually do?”
Explain Pain was Lorimer’s and my first attempt to take the complex pain biology that was exploding in the scientific literature and make it relevant, interesting and understandable. We hadn’t intended to write a step by step ‘how to’ treatment guide – but over the years, we’ve both heard from clinicians (like the one above) who were challenged by the material – and it’s practical application. We’ve never wanted to put forward a formula or a ‘method’ for Explaining Pain, but the idea of another book – a kind of clinician’s ‘manual’ – that went really deep on the neuroimmune biology of pain and how to deliver Explain Pain interventions based on educational psychology and science, has bubbled along in the background. The result of all that bubbling and brewing of course is Explain Pain Supercharged – a book that supercharges your pain biology while also providing chapters on conceptual change science, curriculum development, Explain Pain competencies and assessment, clinical metaphor, and a huge list of ready to use educational neuroscience nuggets and novellas.
A peek under the Explain Pain hood
For this NOInote, we thought it might be useful to provide an example of how it can all come together right at the coal face – as you sit with a person experiencing persistent pain in the clinic. What follows is a taste of Explain Pain in ‘real time’ – it is by no means meant to be a ‘recipe’ for Explaining Pain, but rather a glimpse into our thinking, clinical reasoning and integration of Explain Pain resources. Read on…
Subjective Assessment
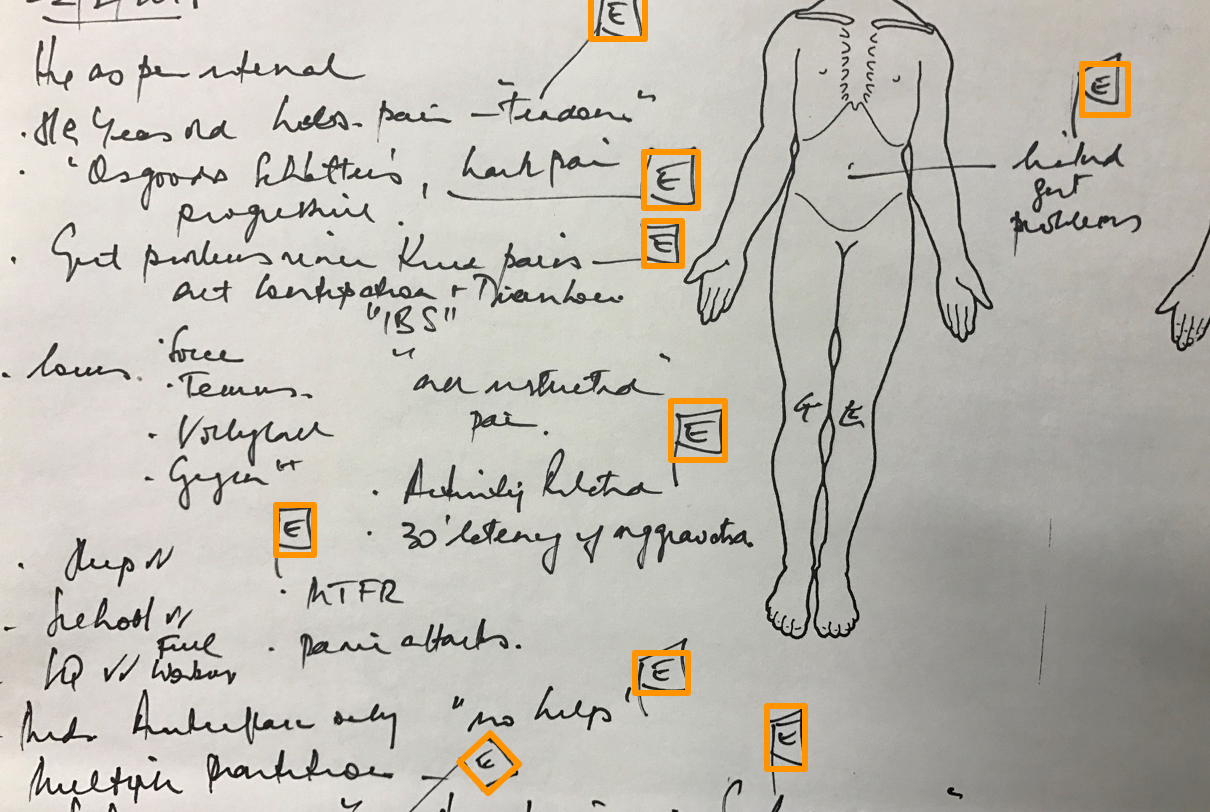
Cassidy (not her real name) is an 18-year-old in her final year at school. She previously loved to play soccer, volleyball and go to the gym and has dreams of being a gym trainer. For the last 3 years she has experienced widespread, bilateral pain (as per body chart below). She has seen multiple health professionals and has been told she has Scheuermann’s disease and ‘will always have pain’ and has been given ‘core stability’ exercises. Cassidy now abstains from soccer and volleyball, is worried about her future, gets down and depressed and has developed gut problems. Some of her family think she is being ‘dramatic’. A full medical work up revealed no red flags.
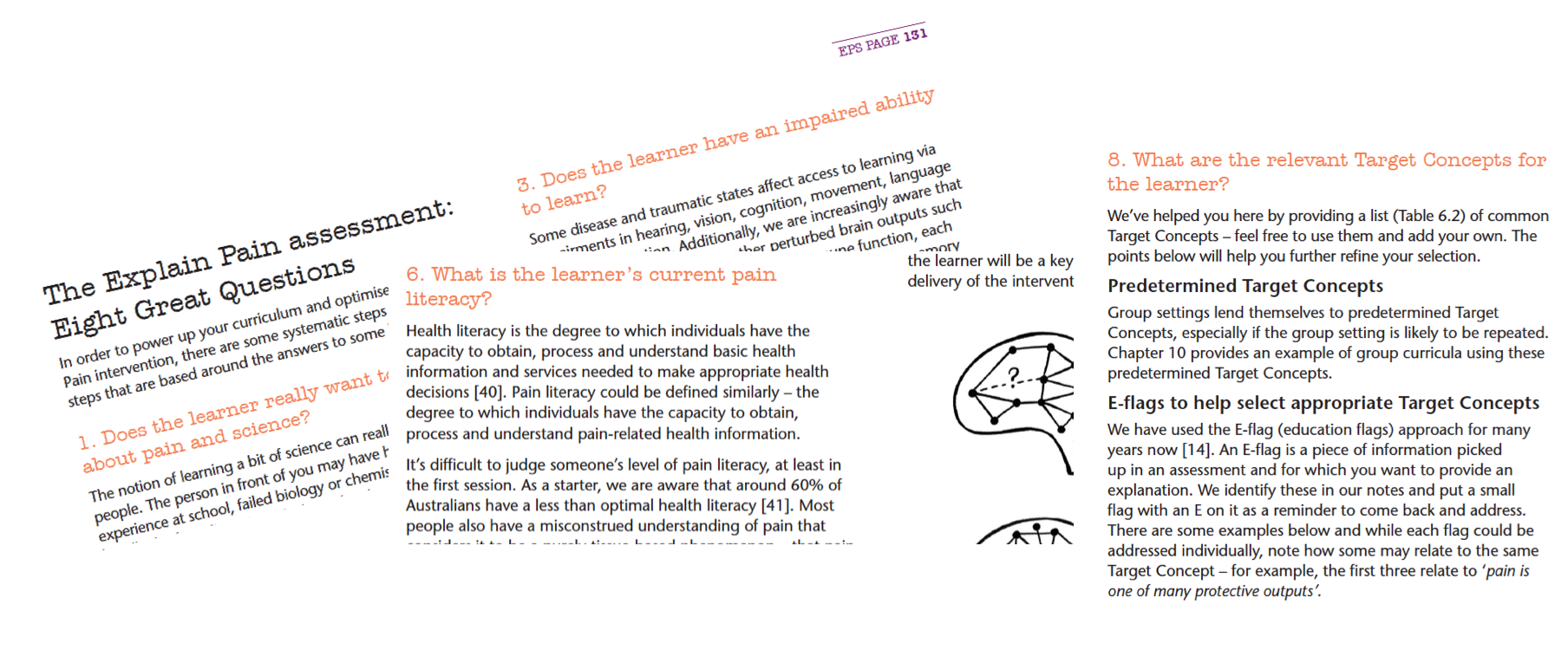
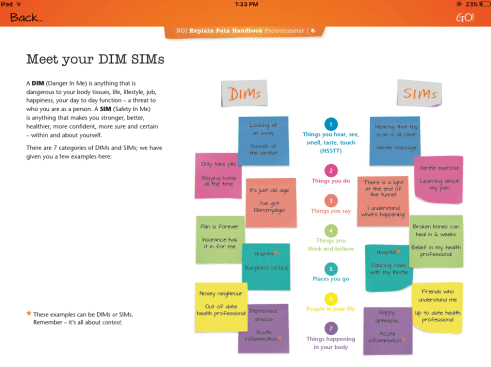
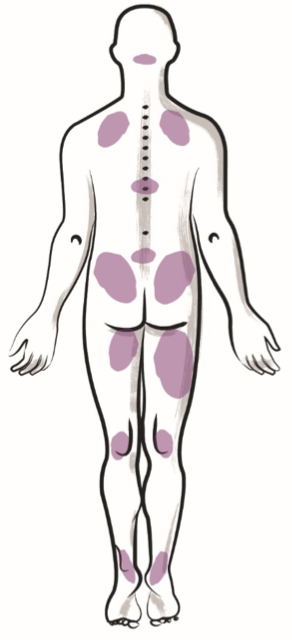 David Butler’s internal thinking and monologue, captured via advance brain scanning*: Lots of E flags (see definition below) here – long term, widespread pain is suggestive of some sensitisation processes and the depression and gut issues hint at multiple output system perturbation. The ‘Scheuermann’s Disease’ diagnosis is potentially a potent DIM driving worry and pain, and needs dethreatening and explanation – probably needs to be a Target Concept.
David Butler’s internal thinking and monologue, captured via advance brain scanning*: Lots of E flags (see definition below) here – long term, widespread pain is suggestive of some sensitisation processes and the depression and gut issues hint at multiple output system perturbation. The ‘Scheuermann’s Disease’ diagnosis is potentially a potent DIM driving worry and pain, and needs dethreatening and explanation – probably needs to be a Target Concept.
Objective Assessment
All spinal movements are a bit limited and shaky. Forward flexion to knees ‘pulls in my back’, and a gentle chin tuck increases this pull. Straight leg raise (SLR) is limited bilaterally to 30o and felt in the knees posteriorly. Bilaterally, slump test is restricted and shaky with thoracic pain on spinal flexion released with knee flexion. All neurological tests are normal except for an excessive knee jerk bilaterally. Lumbar two-point discrimination (TPD) is normal bilaterally. Recognise results of left/right= discrimination in the back and feet are normal.
DB: More E Flags here – the chin tuck increasing the pull in the back would benefit from a neurodynamic story, perhaps with a focus on how growth can affect the permissibility of neural movement. Nothing major objectively, but the increased knee reflex fits with a sensitive system and perturbed outputs. Restricted and shaky movement may indicate that ‘motor control’ and ‘core stability’ approaches are the opposite of what is required – motor freedom on a foundation of up to date knowledge
Explain Pain Assessment
Cassidy is keen to learn about pain and science and prefers to learn via talking, reading websites and watching video clips like YouTube. She gets good marks at school and is studying some science (psychology). Likes to think of herself as a ‘tech-savy millennial’ and has access to a smartphone and an iPad. Her health knowledge comes from teachers at school, talking with friends and family and Facebook ‘news’ articles. Sometimes she looks up conditions on Google. Cassidy doesn’t know a whole lot about pain (low level pain literacy) – ‘I always hurt but I don’t know which part of me is broken’.
DB: The level of misconception (a belief that pain is equal to damage in the body) is likely at the ‘sandcastle level’ – multiple bits or ‘grains’ of information loosely held together; opportunity for conceptual change here. This has likely been reinforced by notions of a ‘weak core’ that needs to be ‘strengthened’. Relevant Target Concepts include 2, 3, 4, 5, 6, 7, 8, 10 and additionally specially constructed Target Concepts ‘Growth spurts and the mobile nervous system’ and ‘The story of Scheuermann’s – it’s not a disease’.
Treatment Day 1
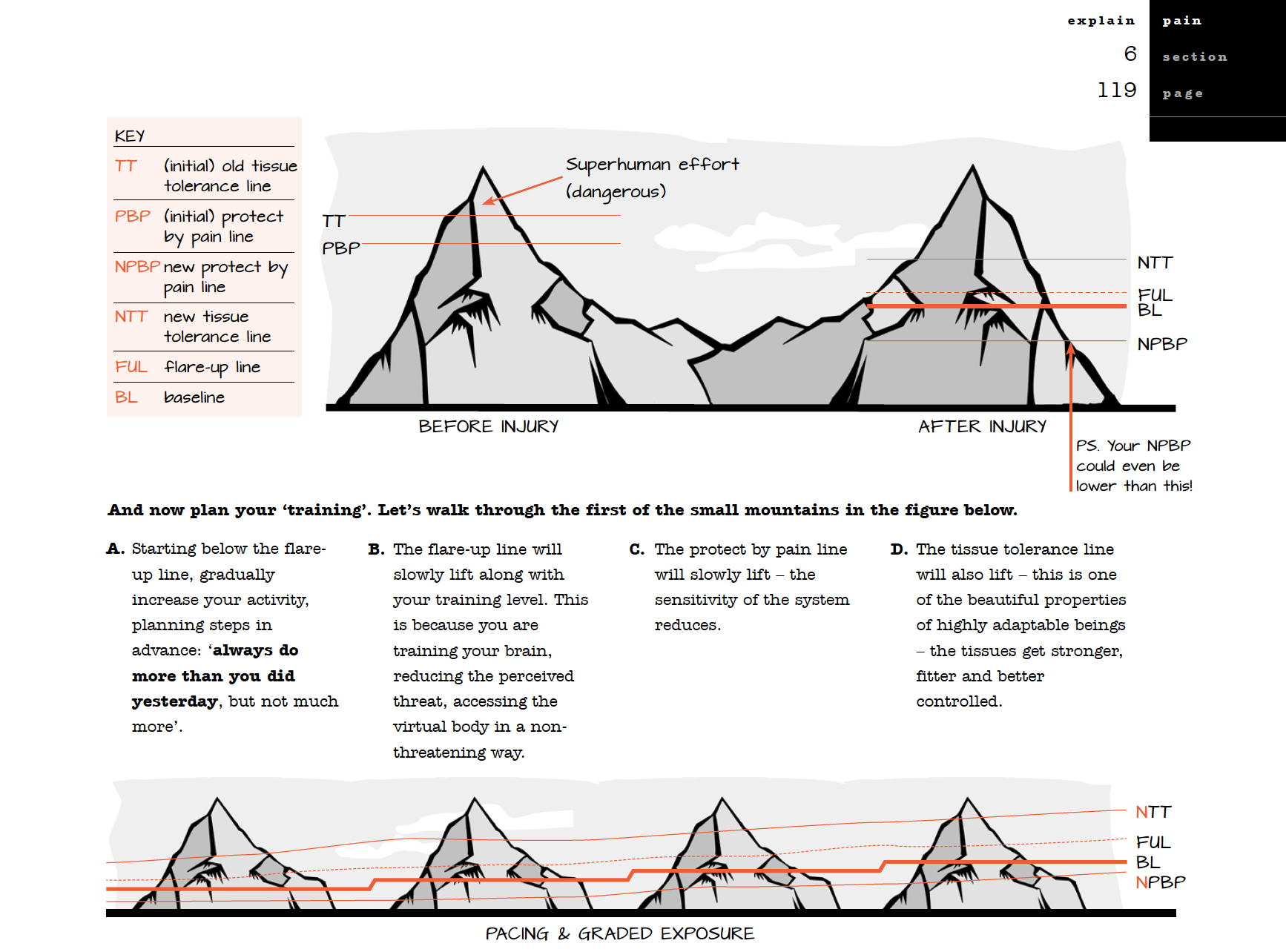
Education: Discussed overprotection using the Twin Peaks Model – exploration of how other symptoms may be overprotective (i.e. pain, gut problems, mood). Introduced the notion that pain and tissue damage aren’t always related. Discussed the bioplastic nature of the nervous system and potential for change.
Movement: Ceased previous core stability exercises. Education provided as to why – discussed outdated notions of ‘motor control’, ‘weakness’ and links to pain. Discussed how updated, dethreatening knowledge could provide new context for motor freedom. Introduced gentle slump/slider movements and graduated spinal flexion with breathing techniques. Discussed the goal of loose, free, easy, comfortable movement rather than being tight – ‘loose and long rather than tight and tense’.
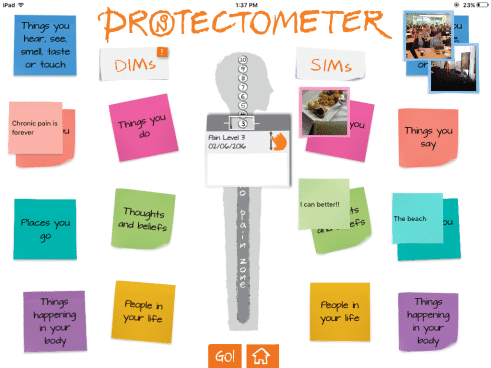
Homework: Provided The Explain Pain Handbook: Protectometer as a guide throughout this journey and encouraged to read page 1-20 and fill in activities. Prefers to use iPad so will fill in ‘Protectometer’ on the App. Agreed to purchase the eBook version of Explain Pain and read ‘Amazing pain stories’ (page 8-17) on iPad.
Plan + Contract:
Discussed the importance of active treatment in both education and movement – agreed on a ‘treatment contract’ with the following objectives to be achieved over next three visits:
- Understand pain biology knowledge as it relates to Cassidy and use this knowledge to change thoughts and beliefs about pain and damage, and move differently with less fear and worry
- Set realistic short and long term goals
- Commence a graduated return to full function
- Use the knowledge and experiences as part of career development
This was covered in a 60 minute initial consult.
To be continued
In a first for NOInotes and noijam, we’re going to deliver a number of serialised posts so that you can follow Cassidy’s progress, and the clinical reasoning that goes with it, over subsequent consults.
Comments? Questions? Sound off in the comments below.
– David Butler & the NOI team
*Not really, he just wrote it down later.
E Flags – An E flag is a piece of information picked up during a routine assessment or a deeper DIM/SIM analysis (Protectometer) for which you want to provide education and explanation. We identify these in our notes and put a small flag with a ‘E’ on it as a reminder to come back and address it later during an Explain Pain intervention.


Lovely. Looking forward to reading more.
Thank you. That’s really useful to see the work in action at the coal face. There’s a lot you can do in 60 minutes!
Awesome!
Really looking forward to more posts.
David, how do you explain Cassidy’s profound state of sensitisation? What would you tell her?
John,
I would like to think that I didn’t tell her anything. But there was a lot of discussing, tempting,planning, perhaps cajoling, sharing , setting up, in a very two way interaction.
More info in the next Installment
David
David, sorry to have “jumped the gun”. But if at the initial consultation Cassidy had asked you for an explanation of her profound state of sensitisation, how would you have responded?
She didn’t and it would be rare for patient ask for an ” understanding of my deep sensitisation”. But if she did I would responded positively with something like “yes over time we can work out some of the things that have likely made you overprotective and sensitive.
More info in next installment
David
Brilliant….helps bridge that gap between understanding theory and really putting it into practice, thank you!
Thank you so much!!!
Thank you so much!!
Really useful post and willing to read the next ones. Is “Explain Pain supercharged” going to be in spanish in the short term? I use “Explicando el Dolor” (“Explain Pain”) with my patients, but I would like yo use the newest book as I consider ir a great tool. Thanks.
Hi Rodrigo,
Explain Pain Supercharged won’t be in Spanish in the short term. But maybe later.
David
I think providing an example for recovery for a “structural” change in bony anatomy is very helpful. Soft tissue pain from a torn ligament or tendon are difficult too but most would assume healing would take place. Scheuermann’s is thought of as a permanent problem and therefore not going to heal and permanent deformity is for life. Well done.
Any chance of protectometer for Android?
I will keep asking for you Aiden!
David
Would you share details of the “long and loose” and the spinal flexion/breathing exercises? I have some ideas but would love to learn from yours too.
Hi Kate,
“long and loose” is simply a metaphorical term that I would use (along with others such as ‘motion is lotion”, “brain is boss”, “get sliding and gliding”) to help untangle the “need for stability” misconception that many people in chronic pain have.
For me, the movements prescribed at first visit are something for the patient to take home, a link and a reminder of the potentially more powerful educational intervention that they have just been through, plus something to remind them that change is possible, as well as movement explorations with a different concept.
David
Brilliant! This is quite an education you are giving to us. To place explaining pain into a constructive framework is invaluable. Thank you for this post. It is very helpful.
Thanks David..looking forward to the next installment.
David- I love it! I really learn from stories like this! It is really instructive to see your clinical reasoning process & how you proceeded through the evaluation. Keep them coming!!! Erica
Hi David I have been using Pain Neuroscience Education for several years now.I work both privately and in the NHS in the UK. I find it a great tool and have found it has taken that time to get across the message in a clear, non confrontational way through metaphors, analogies etc, that I love to update as often as possible to keep it fresh for me.
The big problem I find is that when you are at the start of a revolution you tend to suffer yourself a bit as a practitioner.This is because this is often new information for the patient and, as stated in previous posts, the last practitioner (s) will often be a yellow flag(s) as with Cassidy and the “core strength” which I come up against all the time.It can make you seem a bit of a oddball, with some patients getting the story and others even getting angry, though I do believe my delivery has improved with experience.
My message to all embarking on this exciting journey is keep your ethics and beliefs, but the best advice is to LISTEN.As the excellent blogger Bronnie Thompson says you have to earn the right to educate and that requires listening to their story with as little interruption as possible and to reflect back.It took me a long time to understand this to be the key to the alliance, but even now there is the temptation to jump in to challenge their beliefs, when they say something distorted, that has often been told to them by someone else.
I love my work.I may not get the recompense that all my hard work possibly deserves, but I feel I’m on the right team and have developed a geeky love of my subject.Many Thanks to all you Aussies who are setting the pain field alight.
Hi David, thanks for your great article. Is there any research supporting the “long/loose”, free & easy movement (I realise there’s evidence re the tight and tense)
Cheers!
I hate to be so bold, but I’m loving Peter O’Sullivan on Youtube at the moment. I think he’s your guy.
Thank you Kate. I watched the vids, and think they are great…clear and concise and extremely effective…and he talks about tight and tense not being good (there’s research to support that) and long and loose being good (using David’s metaphors here). He does mention one piece of research that supports “normal movement” unfortunately I don’t know it…do you? I’d like to get supporting evidence of normal movement but specifically “long and loose” – I am a physio but also an Alexander Technique teacher which is all about normal movement and “long and loose” – I just would like to gather more research around the elements of it! Can David offer anything?
Sure – Peter is right on our wavelength!
David
Dear NOI team, dear David,
Absolutely enjoy reading your blog. Thanks for your work and input into that aspect of our practice.
Could you lay out to me the target concept of ‘The story of Scheuermann’s – it’s not a disease‘?
Thank you very much.
Philipp
Hi 🙂 I’m trying to find the follow up posts to this one – did they happen? Thanks so much!
Hi Sally,
No they didn’t. Just me being slack. I will write up the next stages when I am back from holidays. Thanks for checking in.
David
Thanks David 🙂 I look forward to the read when you have time!
Congratulations David!! Wonderfull form of thinking.
I`m returning to NOIgroup, hope to be more connected to all