An epidemic no one talks about
Pain statistics feature at the beginning of every talk or presentation on chronic pain – 1 in 5 people affected, billions of dollars in treatment costs and lost productivity, thousands of hospital admissions per capita, and so on and so on. But the problem with big numbers like these is that they can overwhelm and numb the listener. Prevalence studies and economic statistics have informed us for over a decade that chronic pain is a global problem, and while there are some signs that things are getting better, chronic pain is still a mostly silent epidemic.
You know something John Snow
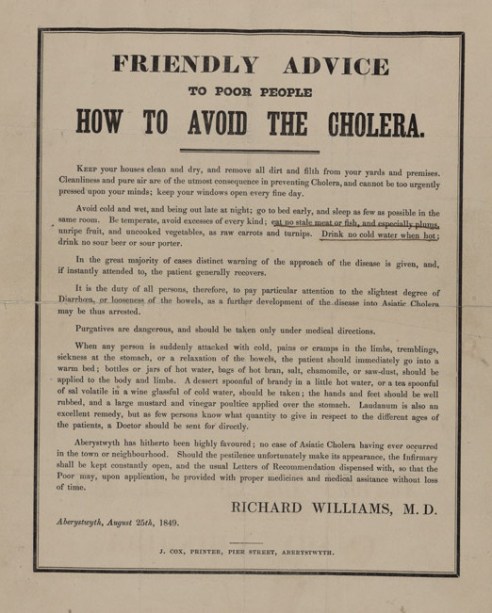
Throughout history, one common factor in dealing with and preventing epidemics has been public education. Check out the ‘Friendly Advice to Poor People’ below. In 1849, the best advice given to the public to avoid ‘the cholera’ was to go to bed early, drink no sour porter and observe ‘the duty of all persons’ to ‘pay particular attention to the slightest degree of Diarrhoea, or looseness of the bowels’.
The discovery by English physician John Snow (not that one) in 1854 that a contaminated public water pump in Soho was the source of a cholera epidemic, was fundamental in changing the public education message. See the poster from 1866 below.
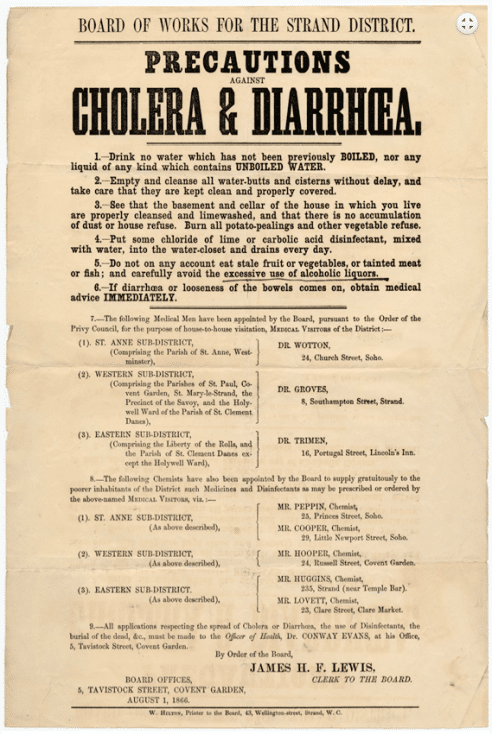
Cholera is still a problem in parts of the world, but it is preventable and treatable – the spread of public awareness regarding sanitation, clean water supplies* and simple treatment with re-hydration has saved millions of lives.
National Pain Week 25 – 31 July
Each year Chronic Pain Australia runs a week long public awareness initiative known as National Pain Week. This year, the theme is fitting with a silent epidemic; Pain – the invisible challenge. Chronic Pain Australia has enlisted Michael Clarke, one of Australia’s greatest cricketers, as an ambassador for National Pain Week and he is using his celebrity and personal experience of chronic pain to encourage people to start talking about the problem of pain
[youtube https://www.youtube.com/watch?v=fVXC4kxXgqs&w=560&h=315]
For more details on National Pain Week check out the website here. Other initiatives with similar goals of public awareness and discourse include the American Chronic Pain Association Pain Awareness Month each September (David Butler has been asked to feature on a podcast related to Pain Awareness Month – keep an eye out via NOI channels for details).
At NOI we agree that with chronic pain reaching epidemic levels, part of the solution has to be improved public awareness and education, and as educationalists, we are all for getting an up to date and accurate message out to all as we aim for a Number Needed to Educate of 1. Below are some of our ideas on how to help get the message of chronic pain out there.
In your face
Prevalence
Sometimes it can be appropriate to get a bit ‘in your face’ when trying to get a message across. Remember those pain statistics up the top, we think they can be given some punch with a few simple tweaks. Based on current figures the number of people living with chronic pain in Australia is equal to the entire population of Queensland – about 4.6 million people. Imagine an entire state, millions of people, where every single individual experiences ongoing pain everyday. Every person you see on the street, on a bus, at home, at work… including you, is in pain almost all of the time. This might get people talking…
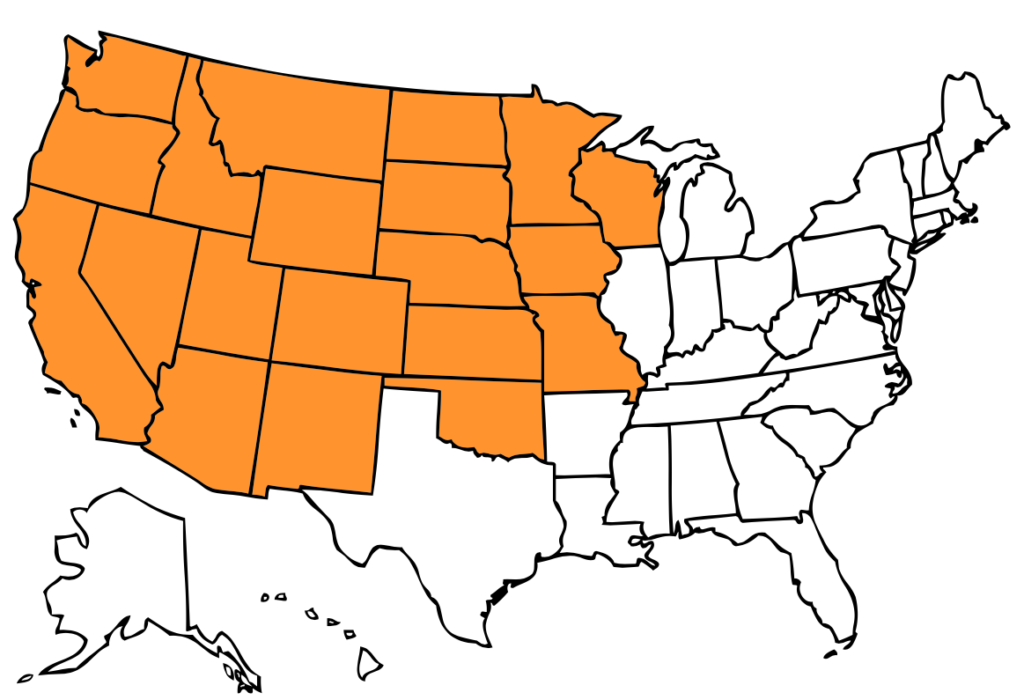
We’ve constructed the following map based on current figures estimating 100,000,000 Americans experience chronic pain and census data on state populations. Imagine every human being in the shaded states experiencing ongoing pain.
Or consider the most recent numbers out of the United Kingdom based on a systematic review which estimates just under 28,000,000 (all those zeroes might help get the point across) adults are affected by chronic pain. This number represents the entire populations of
Greater London + West Midlands + Greater Manchester + West Yorkshire + Hampshire + Kent
It’s also greater than the entire population of Australia – imagine an entire continent where every single person is experiencing ongoing pain.
Cost
Chronic pain is estimated to cost Australia over $34,000,000,000 every year. Our politicians have been squabbling over spending nearly this amount on a National Broad Band Network (which incidentally, if done well, could give millions of people access to the knowledge, information and resources they need to treat pain), yet every year billions of dollars are lost from the economy as a result of chronic pain.
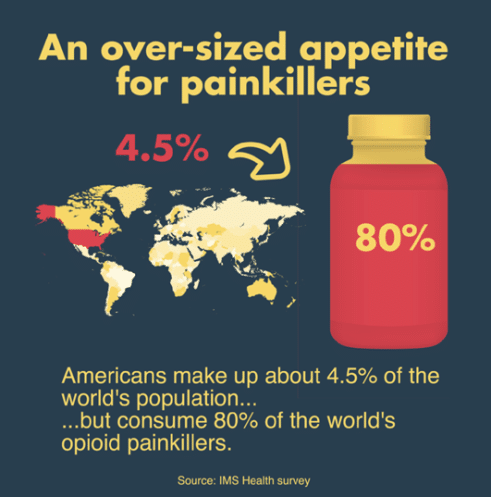
Call bullshit on ‘pain doesn’t kill’
We hear it sometimes, ‘yes, pain is a big problem, but it doesn’t kill people’. Our response is a resounding BULLSHIT. Pain kills people, opioid overdose deaths have quadrupled in the US between 1999 and 2014 with 165,000 people dying over this period. In 2012 70% of all accidental opioid deaths among Australians were due to pharmaceutical opioids.
Do it for the kids and the other ‘missing groups’
Most pain statistics don’t include children and adolescents – these are truly invisible groups in the world of chronic pain. And consider this – in the 1980’s infants were still undergoing open heart surgery with no anaesthesia as it was thought that they didn’t feel pain. But chronic pain affects between 25% and 35% children, especially adolescent girls.
Children aren’t the only missing group – pain is a major problem after stroke and in people with Parkinson’s Disease, multiple sclerosis and other neurological disorders, but it gets hardly any attention.
Go multimedia
Words and messages that are associated with images are more memorable – they’re more ‘sticky’. There are some simple guidelines for effective, evidence based multimedia education, and a good infographic can make a strong point with very few words
Get personal
Punchy statistics can have their place, but they can still be hard to relate to. Chronic Pain Australia have enrolled Michael Clarke’s as an ambassador to tell his personal story, and perhaps even a few might hear what he has to say and think, ‘if he can talk about pain, then so can I.’
When people are encouraged to tell their story, and given the time and space to do so, the words that flow can often have an arresting effect. Consider these statements recorded as part of a phenomenological analysis of the personal experience of chronic low back pain
‘When you don’t feel you have a future, you live in the past.’ Rachael
‘I’m sort of mad at myself I start banging things and getting so aerated with myself that it’s there and I can’t get it to go away.’ Linda
‘But I don’t know why you have to keep suffering it and suffering it and suffering it for ever and ever.’ Becky
Perhaps sharing some of these experiences as part of your next talk with health care providers, insurers or other stake holders will help get the message across.
Remember that DIMs and SIMs hide in hard to find places.
The idea of pain as a silent epidemic fits perfectly with the idea that ‘DIMs and SIMs hide in hard to find places’. We’ve found consistently that sources of ‘Danger In Me’ can be as invisible as pain itself, but appropriate Explain Pain and careful use of the Protectometer can help uncover these sources of threat in the world.
Perhaps some of the most powerful SIMs that an up to date, globally aware and socially engaged health professional can provide to a patient is the knowledge that the problem of pain is being acknowledged, and that there is hope for better treatment and outcomes.
So join the Explain Pain revolution – support the awareness weeks and months online and in your community, get out in the world and get vocal, because if there is anything that Jon Snow has taught us it’s that knowing nothing is no longer an option.
Add your voice in the comments below.
-Tim Cocks and David Butler
*The lack of clean water and sanitation is tragically still a major problem in parts of the world – there are many organisations that are working to end this problem – wateraid.org is just one of them.
![aussie_tour_banner_2016[1]](https://noigroup.com/wp-content/uploads/2020/11/aussie_tour_banner_20161.jpg) Last chance to get on an Australian Explain Pain or Graded Motor Imagery Course for 2016
Last chance to get on an Australian Explain Pain or Graded Motor Imagery Course for 2016
Gold Coast 30 September – 2 October Explain Pain and Graded Motor Imagery (Close to full, remaining tickets selling fast)
Perth 15 – 17 October Explain Pain and Graded Motor Imagery
EP3 events have sold out three years running in Australia, and we are super excited to be bringing this unique format to the United States in late 2016 with Lorimer Moseley, Mark Jensen, David Butler, and few NOI surprises.
EP3 EAST Philadelphia, December 2, 3, 4 2016
EP3 WEST Seattle, December 9, 10, 11 2016
To register your interest, contact NOI USA:
p (610) 664-4465
e noius@noigroup.com



An amazing, eye-opening document. Thank you!
Thanks Mary. We hope it encourages conversation and even better – action.
My best
Tim
Hey Guys, by using cholera as an analogy, you seem to be suggesting that not only is “chronic pain” a distinct disease, but also that medical science will eventually come up with a cause and a cure. But I feel sure that this was not your intention.
The other point worth discussing is whether or not we really are seeing a modern day epidemic of people with chronic pain. If we go back a century or so, many of those with chronic pain in the English-speaking world would be found amongst the large numbers of people who were then being awarded such fashionable but nebulous labels as “fibrositis,” “muscular rheumatism,” “neurasthenia,” “railway spine,” and “occupation neurosis”.
Hi John
Thanks for dropping by. Correct, not our intention, but I can appreciate that some might see that link. Cause and cure are two rabbit holes too fraught to explore with my limited understanding of pain.
Definitely a point worth discussing. As Allan and Waddell said nearly three decades ago:
“There has been an epidemic of low back pain since World War II. Or, more accurately, an epidemic of low back disability (Waddell 1987). But back pain is not new. So what has changed about back pain? In this paper we will try to put this epidemic into historical perspective.”
“Despite a wide range of treatments, or perhaps because none of them provide a lasting cure, our whole strategy of management has been negative, based on rest. We have actually prescribed low back
disability! Modern medicine has not solved the problem of backache (Waddell 1987). Instead changed patient attitudes and expectations, changed medical ideas and management and changed social provisions have all combined to cause low back disability”
‘An historical perspective on low back pain and disability’ Allan DB and Waddell G (1989) http://www.tandfonline.com/doi/pdf/10.3109/17453678909153916
A challenging read.
Best
Tim
Thanks Tim. Theirs was a pivotal paper but if I remember correctly, Allan and Waddell were only discussing chronic low back pain. What about the rest of the “foul rheumatic breed”?
Hi John
Yes Allan and Waddell focus on low back pain, but my reading has been that LBP was chosen as a vehicle (somewhat of convenience) to discuss issues of public attitudes and understanding, and societal influences, on pain and disability, rather than the paper being ‘about’ back pain per se.
Has the health/medical professions’ engagement with the “foul rheumatic breed” been any less iatrogenic?
Granted, the question of what exactly is at epidemic levels, is certainly a valid one.
Best
Tim
Tim, it is too easy to play the “iatrogenic” card when the real problem might be that medical science has not provided the wherewithal for us to fully understand the biological mechanisms responsible for these painful conditions. Of course, public attitudes and societal influences have always loomed large in determining questions of disability. This is why the Faculty of Pain Medicine, ANZCA, has “flipped” the pain curriculum, replacing Bio-Psycho-Social with Socio-Psycho-Biological. Unfortunately, lip service continues to be paid to the former, which was only ever a framework for discussion between clinician and patient and never a scientific model.
John, the easy card doesn’t mean it’s necessarily the wrong card! But I take your point. Equally, iatrogenic does not need to be entirely pejorative – I think we all proceed with the very best of intentions towards those people experiencing chronic pain, but it is the very lack of wherewithal that can make our interactions more harmful than helpful. I’m very aware of my time genuflecting to the emperor the Intervertebral Disc, whose dynasty has wained, but not altogether faded. Strangely enough, more than a few patients seemed to achieve remarkable results with repeated McKenzie extension in lying, a lumbar roll, a few days with a bit of anti-flexion rigid sports tape and a copy of Treat Your Own Back…
Do you think that conditions belonging to the foul breed require special explanation? I must confess to not knowing enough about these conditions to comment further, at the same time as feeling that ‘rheumatism’ might be a beetle in a box as we converse.
What are the prospects, do you think, of the SPB framework becoming a scientific model? Does it need to ?
Enjoying the chat,
Tim
Tim, it appears to me that the individual members of what were once referred to as the “foul rheumatic breed” have been subsumed by the catch-all term “chronic pain”.
As I have come to understand them, useful scientific models of the real world should both explain and predict phenomena of interest. Neither BPS nor SPB were formulated to fulfil these conditions.
Thanks John. Does it matter? What shall we call it? Hopefully not “central sensitisation syndrome” or “central sensitisation pain” as I’m seeing more and more of in varying guises and syntax. This new reification of plastic changes in the dorsal horn has already reached patient vernacular, evident from emails we receive.
From a very (some might say overly) pragmatic perspective, the subsumption you mention has added power to the statistics. There may be some political/funding/societal awareness benefit from this. Too Machiavellian?
Best
Tim
Does it matter? What shall we call it?
Tim, I am reminded of this observation made by William Heberden [1710-1801]: “The rheumatism is a common name for many aches and pains, which have yet got no peculiar appellation, though owing to very different causes.” Reference: Commentaries on the History and Cure of Disease, Ch. 79.
IN 2007–08…
In Australia, 67% or 11.1 million people aged 15 years and over reported experiencing bodily pain in the previous four weeks. Around one in ten (9%) Australians experienced severe or very severe levels of pain.
More Australian adults experienced chronic pain in 2007–08 than in 1995. Rates of overall body pain for people aged 18 years and over increased from 57% to 68%, while severe/very severe pain increased from 7% to 10%.
Source: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4841.0Chapter12011
I am not an epidemiologist but the following extract may be of more than historical interest:
“Two points need special consideration: (1) that the total number of rheumatic sufferers includes those who are affected to only a minor degree, not badly enough to consult medical advice or stay away from work: these can be gathered into a statistical record only by direct contact with the persons attacked; (2) that satisfactory diagnosis of the type of rheumatism cannot be made by the person attacked, and in many instances not even by the doctor in general practice; ancillary aids available only in special centres are required.
There is a real problem involved in spreading a net sufficiently wide to catch all degrees of severity and subjecting them, even those of mildest degree, to the most modern diagnostic procedures.”
Reference: Lewis-Fanning E. Incidence and prevalence of adult rheumatism. In: Fletcher E, ed. Medical Disorders of the Locomotor System. Edinburgh: E. & S. Livingstone Ltd. 1947: 98-119.
Thank you for writing this article. I’ve just had a horrible experience with my pain condition (I’ve had crps and now have lots of central sensitisation – my body is very unpredictable in how it responds to pain events). I’ve just had some surgery. My pain specialist wrote to him about my condition prior to surgery. Most nurses didn’t understand why I needed a ketamine infusion post surgery carpal tunnel and ulnar release surgery. After the infusion was stopped the doctor discharged me as my pain was quiet. Whilst waiting for some meds from the pharmacy my pain rapidly increased despite taking oxycodone. The doctor still wanted to discharge me from hospital and just take the oxycodone as the pain would settle within 24 hours (post the nerve block wearing off). I was distraught at the thought of leaving the hospital in pain that was increasing and had reduced me to tears (and I have a very high pain tolerance). I couldn’t get the doctor to understand that a not very painful surgery for the average person wasn’t for me and I needed more help.
In this state I rang my pain doctor who immediately took my call and rang the surgeon on my behalf. Thankfully between the two of us we mangaged to get the message through and since then (to his credit) the surgeon has been wonderfully supportive and ordered different medication and my pain is under control.
I just wish there was a way to get others to better understand my condition and have my pain treated seriously (this is the third time I’ve had difficulties with surgeons and getting them to understand despite the information given to them from my pain doc).
I would love to help to get the message out there about chronic pain and pain conditions so others don’t have to go through this, especially those without an amazingly supportive pain doctor.
Reblogged this on videnomsmerter and commented:
Kroniske smerter i tal…
Thanks for the post Tim.
Interesting aside – John Snow was at WOMAD this weekend and looked like he was enjoying himself immensely. Also, the John Snow is a lovely pub near the original standpipe and definitely worth a visit next time you’re in London. Cheers, Tim
Excellent article.
I note all the interesting philosophizing in some comments above.
I have a coalface view in the compensation world which confirms that it is a serious (and expensive) problem whether considered a new epidemic or not. There are commonly repeated scenarios with tragic circumstances in many individuals as it is abundantly clear that the context of a pain event dictates the outcome, not the severity of the mechanism or the discovered ‘pathology’. Iatrogenesis is the rule through an industry that seems to unflinchingly and consistently misinform that tissue change and pain correlate well, and then treat patients’ bodies like dart boards hoping to hit a target etc, etc.
You use cholera to convey a message. I offer a similar metaphorical message for the interpretation and then communication of ‘scans’ to patients in pain. This metaphor refers to the ‘common cold’ and the use of antibiotics over how many decades …?
Thanks for the informative article on pain. I thought the Cholera before & after comparison illustrated well the difference of awareness based on supposition and awareness via increased understanding of the source of the problem. The other group that might not be included in the 1 out of 5 is the with pain but undiagnosed or the presentation of pain doesn’t follow a ‘known’ pathway or attacks random sites. The latter two being dismissed as ‘all in the head’ & therefore a mental issue; or the person wishing to scam the system – meds/narcotics/attention etc etc, unless the physician is observant and looks beyond that.
Severe pain will often isolate people from society, after a while they stop visiting doctors, not because they are better or a lot better but because the increased pain on movement/draining of what little energy they have/don’t wish to be further stripped of their integrity and the upset or depressive states that follow. Therefore, in addition to the conditions that have been also commented on by others to this article, pain’s true impact could conceivably be a lot higher than 1 in 5.