Reflections on EP3 at the G
I had the fantastic opportunity to be invited to attend EP3 at the G (Melbourne Cricket Ground) as a science correspondent. One of the standout learning experiences was due to the generosity of a gentleman named Russell who donated his time to stand on stage and be examined by Peter O’Sullivan in front of 250 people! Russell’s 35 year story exemplified the discrepancy between guidelines based care and clinical practice.
Evidence base in persistent low back pain
The recent Lancet series in low back pain described this gap between clinical practice and the recommendations promoted in best practice guidelines (Foster 2018). International guidelines in the management of people with persistent low back pain are aligning towards common themes that all health care professionals and the general community need to become familiar. Promoting high value care such as education, returning to usual activity, exercise and cognitive behavioural therapy are recommended (Foster 2018). But education also has to be evidenced based! Unfortunately, Russell clearly described, the journey into persistent disabling low back pain which seemed to be driven by well meaning, but unhelpful and inaccurate healthcare messages as well as societal beliefs (Caneiro 2018, Bunzli 2013).
The three themes of EP3 were pain neuroscience, behavioural science and education. They are the pillars on which we can confidently promote the Lancet series high value care recommendations for persistent disabling low back pain which are:
- Educate
- Promote usual activity
- Graded exercise and cognitive behavioural therapy
Communication during Russell’s consultation
Cognitive Functional Therapy is a model of individualised care that integrates the three high value care recommendations included in the Lancet series. Peter went about his consultation with knowledge of these recommendations, with a solid foundation in pain neuroscience and expert communication skills discussed by Lorimer Moseley and David Butler throughout the conference.
Peter went about discussing Russell’s understanding, thoughts and feelings about his back pain, hearing his story, his use of metaphors and validating his experience. The consultation revolved only around valued activities such as being physically active, playing with his grandchildren, and contributing at work. Pete tested Russell’s beliefs and behaviours by providing evidence based messages, addressing his use of negative language and reducing his fears about moving and loading his body in a way that did not bring on his symptoms. Throughout the consultation, you could see that Peter is truly unafraid of pain. Being calm, confident and empathetic with someone in pain, conveys strong ‘Safety In Me’ (SIM) messages.
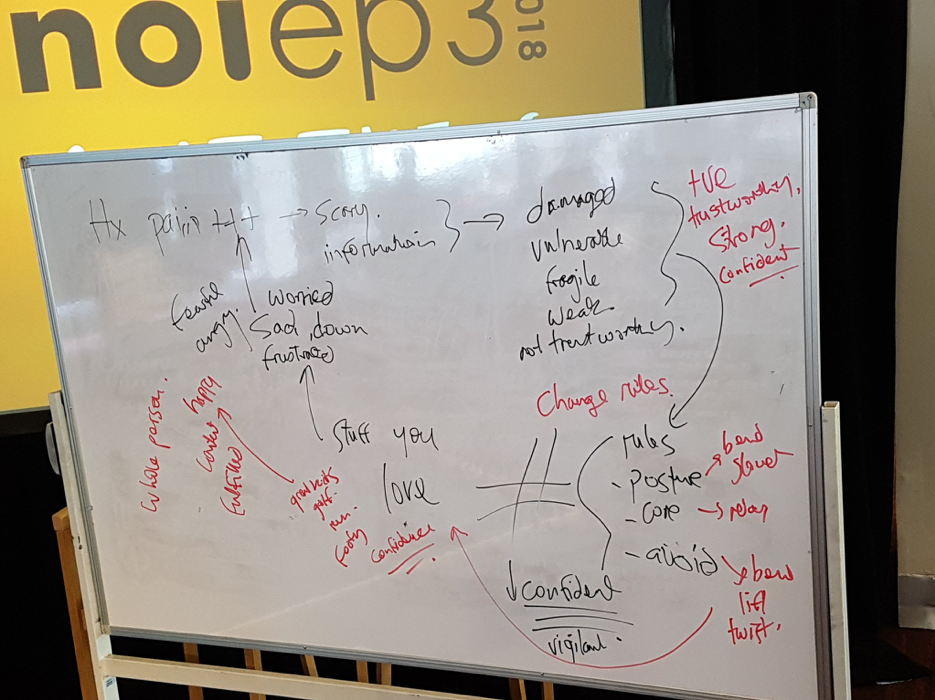
By the end of the consultation, Russell volunteered that he had had changed his mindset about his pain and disability to a belief system consistent with the guidelines. Russell took away messages that replaced “danger in me” language with “safety in me” language. Importantly Peter provided Russell a plausible written schematic about the drivers of his pain and disability (Picture above) that included danger and safety language. A clear path away from pain and disability was described both verbally and visually (Figure 1. Red text – “safety in me” neurotags) that included a contemporary view of pain science.
Communication strategies discussed at EP3
I developed further understanding of 3 key factors that I can immediately apply to my clinical practice:
1. The importance of metaphor
Learning about the use of metaphor as a teaching tool was one of the most exciting components of the EP3 conference. Russell used metaphors “every day when I wake up I am thinking about the back” (disembodiment), “I freeze and start to worry” (journey), “I was told my discs would crumble” (ontological), “wear and tear” (invasive). Metaphors can be safety or danger messages. Ensuring consistent safety messages (Stewart 2018, Darlow 2018, Bunzli 2013) throughout a consult can de-threaten the experience of pain.
2. Reflective questioning
Hear the words that reflect thoughts, emotions and behaviours. Ensure you understand their interpretation of the word. Probing a patient’s thoughts immediately during a consultation allows you in to their story to understand their perspective. If you understand how your patient constructs their language about their pain and disability, you can challenge their beliefs in a non-judgemental manner, and use your understanding of metaphor and cognitions to change misconceptions.
3. Building a curriculum
After you understand your patient’s experience, and understanding, you are ready to build the curriculum for their way out of disability and pain. It’s your job to rid them of unhelpful and incorrect understanding of their problem by confronting their mental model in a respectful manner. Then fill in the gaps with contemporary pain science. Russell was provided an evidence based curriculum during the consultation, summarised in Figure 1. Pete developed the curriculum over his years of practice, and research addressing key curriculum building factors discussed by David:
- Perform a comprehensive and professional appropriate assessment;
- Be truly biopsychosocial (deep in your guts);
- Justify biological literacy inquiring about the potential pain mechanisms (See Mitchell 2018 – Clinical translational framework);
- Have declarative (things you can state) and functional knowledge (things you can do)
- If the person in pain has a linear or emergent mental framework
- Know how to target common concepts including: pain does not equal damage, threat perception facilitates pain, pain involves distributed neural networks, humans are bioplastic, and provided active and self-managed treatment strategies
- Be aware of pain misconceptions
- Develop a personalised Explain Pain taxonomy
Adapted from Explain Pain Supercharged (2018) Moseley GL and Butler DS. Noigroup Publications, Adelaide.
Nuanced Communication
Some comments from the crowd I heard during EP3 were along the lines of: “that’s a lot of detail to teach a patient”, “I’ve tried discussing psychosocial issues, but I don’t get anywhere like Pete does” or “I can’t use the language that David uses without coming off like an eccentric flamingo”. It is our job as health care professionals to use our knowledge of pain psycho-socio-neurobiology to allow us to connect to our patients. The beautiful thing about communication is that it is individualised. Both to you, and the person in pain. We all have our own language, we don’t necessarily have to try to be David, Peter or Lorimer. Using language that is comfortable to both the clinician and the person in pain is very important. EP3 provided me some exceptional insights, broadening my knowledge about the nuance of communicating with a person who has pain related disability.
Part II of this blog [look out for it tomorrow, ed.] will carry on from this and discuss the process of change in Russell as interpreted by fellow Curtin PhD student Kevin Wernli.
-Jay-Shian Tan
 Jay-Shian Tan is PhD candidate at Curtin University, an Australian Physiotherapy Association Titled Musculoskeletal Physiotherapist and Chair of the Musculoskeletal Physiotherapy Australia WA Chapter. He has completed his MSc Clinical Physiotherapy (Musculoskeletal Major) and teaches at both undergraduate and postgraduate levels. Jay consults at Flex Physiotherapy in Murdoch Western Australia with people who have persistent upper limb and spinal pain. The title of his PhD is: Movement and Wearable Wireless Movement Sensors in Knee and Back Pain.
Jay-Shian Tan is PhD candidate at Curtin University, an Australian Physiotherapy Association Titled Musculoskeletal Physiotherapist and Chair of the Musculoskeletal Physiotherapy Australia WA Chapter. He has completed his MSc Clinical Physiotherapy (Musculoskeletal Major) and teaches at both undergraduate and postgraduate levels. Jay consults at Flex Physiotherapy in Murdoch Western Australia with people who have persistent upper limb and spinal pain. The title of his PhD is: Movement and Wearable Wireless Movement Sensors in Knee and Back Pain.


comments