Jay-Shian Tan was a science correspondent at last year’s EP3 at the ‘G. He wrote a stellar blog post about his thoughts on integrating explain Pain and Cognitive Functional Therapy and has followed up with another post focussing on his PhD studies. This one should challenge some thinking!
Late last year I was asked to commence a PhD under the guidance of 5 superstar supervisors: Associate Prof Peter Kent, Dr Amity Campbell, Professor Anne Smith, Professor Peter O’Sullivan, and Dr Joao Paulo Caneiro. While I am told 5 supervisors is not the norm, and has the potential to result in conflicting messages, my team is full of trusting and caring people who have strived together to support me every single week since I started my studies.
EP3 at the G (Melbourne Cricket Ground), was my idea of heaven. A bunch of clinical and research nerds, raving on about pain science is my happy place. So… pain science, what is that? Well I think it’s anything to do with pain…anything and everything.
You might be thinking, “You’re in Pete O’Sullivan’s group, you must be investigating how people think and feel”. Well, let me tell you, of my 5 supervisors, all have extensive experience in biomechanics, you heard that right…BIOMECHANICS.
Yes, that’s right, our group still feels that biomechanics is an important component of the puzzle in the management of persistent pain conditions such as low back pain and knee osteoarthritis. Movement is a behaviour, behaviour can be changed, and therefore we can affect movement by changing how people understand their pain. With the use of appropriate language and developing an individualised curriculum, which might include biomechanical information, people can be assisted back towards their valued activities which they have been avoiding due to fear and/or pain.
My studies involve the use of inertial measurement units. “What the hell is that?” you might ask. Well, these are sensors that are in such things as your mobile phone which can help provide information on movement and orientation data. With two sensors, we can determine a joint angle and speed (kinematics), and the particular sensors I will be using also include a surface EMG which measure muscle activity.
Research has clearly shown that people with musculoskeletal pain disorders display consistent alterations in key movement domains: they move with less range of movement, move more slowly, and have higher levels of muscle activity compared to people without pain (Laird 2018, Geisser 2004, Laird 2014, Hicks-Little 2011).
My PhD uses the exciting new inertial measurement unit technology to help determine if:
- People with knee OA move similarly at home compared to in a laboratory setting.
- We can track changes in how people with knee OA move over the course of a CFT intervention, and if it relates to changes in activity limitation or pain
- A change in movement is associated with a change in activity limitation or pain in people with low back pain
Over the course of the EP3 conference, I was asked the question, “So when is movement important?”. My clinical brain gives me the ambiguous answer “when it is”. The open access article by Laird 2018, shows 4 distinct subgroups of how people with and without low back pain bend (Figure 1).
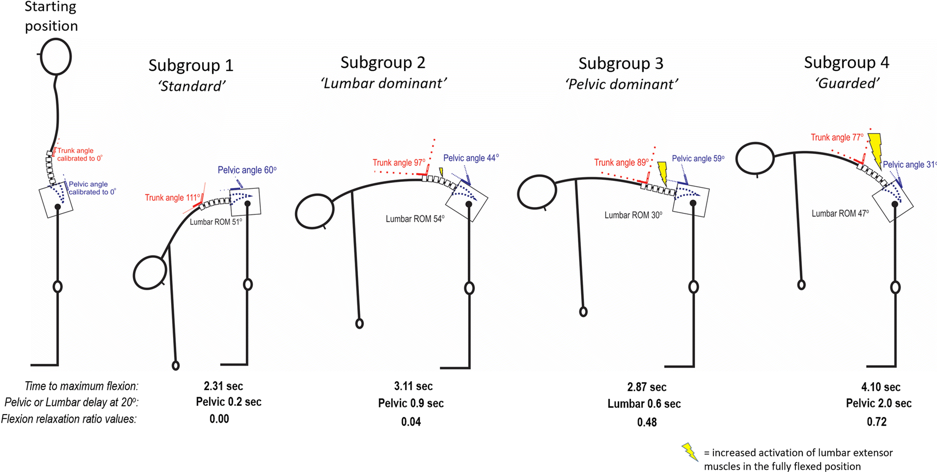
Figure 1. Laird et al 2018
I hypothesise that people in subgroup 1 need no changes in their kinematics or muscle activity, while subgroup 4 would benefit from reductions in their muscle activity and assistance in gaining ROM. This might come from some important factors such as the safety messages delivered to the patient which can reframe their cognitions (Explain Pain) and behaviours (Cognitive Functional Therapy). While others might improve from some form of technologically enhanced therapy such as normalising EMG or kinematics (inertial measurement unit biofeedback). Multiple research groups are aligning towards common themes in the management of musculoskeletal pain conditions, perhaps one day we will see technology such as inertial measurement units be part of the picture to facilitate guideline recommendations to promote usual activity and exercise, within a comprehensive biopsychosocial model of care.
-Jay-Shian Tan
 Jay-Shian Tan is PhD candidate at Curtin University, an Australian Physiotherapy Association Titled Musculoskeletal Physiotherapist and Chair of the Musculoskeletal Physiotherapy Australia WA Chapter. He has completed his MSc Clinical Physiotherapy (Musculoskeletal Major) and teaches at both undergraduate and postgraduate levels. Jay consults at Flex Physiotherapy in Murdoch Western Australia with people who have persistent upper limb and spinal pain. The title of his PhD is: Movement and Wearable Wireless Movement Sensors in Knee and Back Pain.
Jay-Shian Tan is PhD candidate at Curtin University, an Australian Physiotherapy Association Titled Musculoskeletal Physiotherapist and Chair of the Musculoskeletal Physiotherapy Australia WA Chapter. He has completed his MSc Clinical Physiotherapy (Musculoskeletal Major) and teaches at both undergraduate and postgraduate levels. Jay consults at Flex Physiotherapy in Murdoch Western Australia with people who have persistent upper limb and spinal pain. The title of his PhD is: Movement and Wearable Wireless Movement Sensors in Knee and Back Pain.

Nice one 👍