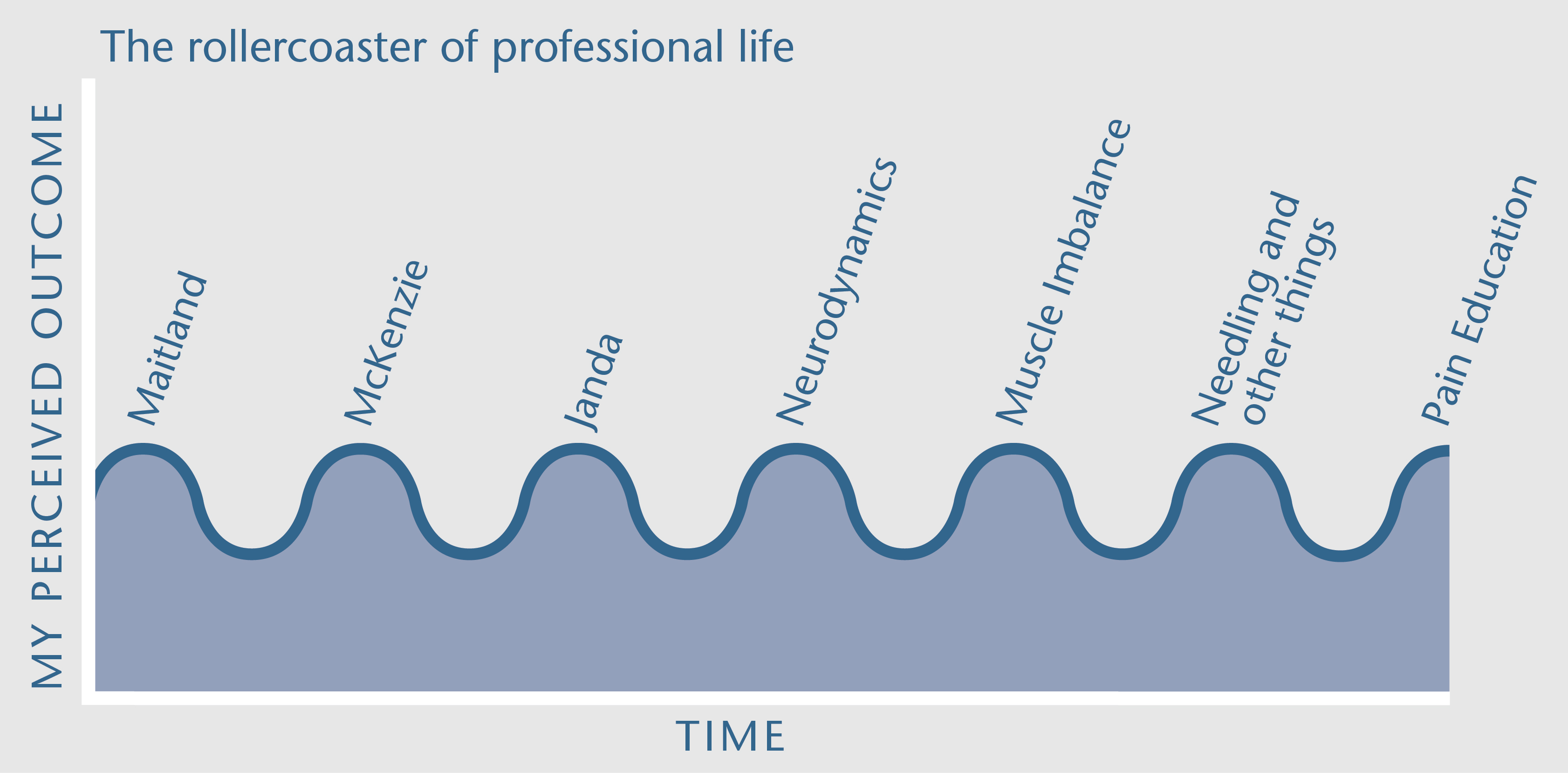
NOI Notes always generate responses which we all enjoy but there has never been a response like the one to the recent Rollercoaster of Professional Life. There were hundreds which included many first time responders and they are still coming in. The Rollercoaster NOI Notes was an observation of the ups and downs of my professional life as I took on new ways, systems and gurus then discarded them, taking the good bits and finally belatedly realising that much of the outcome depended on features of me, not a system or technique. My rollercoaster is summarised below.
I want to summarise the responses and share some of the words of wisdom that came back. It occurs to me that the rollercoaster may well be linked to professional burnout – a problem in all professions and one where research is limited.
Most of us are on a rollercoaster Most respondents said “hey that’s me too”. Even some recent grads were noting it too, but were pleased they weren’t alone. It makes me realise that this should be mentioned in undergraduate education. And I am glad the story made a few laugh! But when you do get sucked in by something and you realise it, it is probably healthy to laugh. Some thought I was at the end of the rollercoaster and retiring, thus the odd mini obituary (thanks for the nice words) but this is not true, I have a few potential waves still left in me! Some younger respondents were relieved that there probably is no holy grail. And some too became aware of colleagues stuck on just one wave (eg “all they do is needle” or “they just go straight to iliopsoas”). A couple had found happy and fulfilling waves along the way with Feldenkrais. I think it helps to contemplate the waves – and as Mike says – “many thanks” and “I will remember this, the next time I become disheartened and want to be a plumber”.
Rollercoaster awareness and unpleasant memories The notes did evoke unpleasant memories for some who recall visiting gurus as patients and being shouted at because they didn’t get better. I too recall lectures where you felt you could not question a particular guru. No wonder things cycle! The notes got regular responder Cameron going – he asks “did any of my lecturers at university ever question a single assumption about any of these so called treatments?”. Being a lecturer back then, I guess, the answer is “probably not – sorry Cameron, we were sucked in”. Cam goes on to say “people are afraid of the truth – that the mind not only creates pain and injury and illness but it literally creates the whole world”, but that is a longer discussion we can have later on NOIjam.
Advice on flattening out the bump and limiting burnout Positivity presented in the responses. As many respondents noted, as long as we are still curious, our jobs will be a pleasure. (Remember to evoke curiosity in your patients as well!). Nicole has a lovely line – it is the challenge of not always being right and thus having to think about and dive into the ever larger wealth of knowledge that helps. Ernst comments that if rollercoaster recognition helps us sense our role and the power of the patient therapist relationship, new ways to treat should lead to reframing of patients’ behaviours and novel coping styles should emerge. I enjoyed Allyssa’s rollercoaster – from transversus exercises to muscle energy to nutrition medicine to the visceral world and how just like in my experiences, each new approach initially appeared to be the answer. “Is it that I convey the placebo response to the patient because I am so newly overconfident after each course but after it is apparent it’s not the whole answer, they pick up on my doubts and the placebo is no longer transmitted.” Probably yes if placebo is taken as brainpower. Craig has had a rollercoaster too but his physiotherapy practice has been helped by studying an MBA – leadership, ethics, marketing, motivation, teamwork, sales etc. Much like Allyson who has found support in Napoleon Hill’s “Think and Grow Rich” and Cameron in Jed McKenna’s “Theory of everything”. Professional improvement and burnout buttressing may not necessarily emerge from yet another rehab course. The rollercoaster notes made some think quite laterally and deeply – Lezanne comments “it is clear my own wellbeing has an effect on patients” and coins the useful phrase “therapeutic use of self”. Deena brings up the issue that the rollercoaster context has changed and we now have to deal with pain systems increasingly bullied and tormented by policy makers. She asks whether bullying has any influence on pain (I don’t know but it probably does). Perhaps Helen sums it all up by suggesting our job is essentially one of being a facilitator of change.
A final wave I have been on my final wave for nearly 20 years now. A few people asked me what my next wave is. There is none. I am convinced that treatment foundations which combine modern neuroimmune science, education science, reasoning and evidence based movement enhancing strategies are the go – all what we teach at NOI. Thanks again for such a response and messages of support. We have enjoyed them all here at NOI.
David Butler, Noigroup

I have been riding the NOI wave for those twenty years too and I agree that this wave will carry us way into the future. Who knows what the next frontier might be but I am convinced that it lies within the brain and the thoughts feelings and emotions that it creates. Or is it the other way round ……?
I agree with Helen that we are the facilitators of change, both within our patients and ourselves. We are back to those three classical clinical reasoning questions:- What do we believe to be the processes at work within this person. What has to change within this person to improve their quality of life. How do we, together FACILITATE that change…..
Again my deepest gratitude to the NOI and the gift it continues to give to the world of pain, suffering and disability ……
To: David Butler
From: Deborah R. Brandt
Re: NOI Notes November 2013, Roller Coaster of Professional Life; “… However the interactional power needs better analysis and understanding …”
Re: NOI Notes Jan. 2014.
Lezanne: “… coins the useful phrase, “therapeutic use of self”.
Helen: “… being a facilitator of change.”
Greetings,
Your November posting and your recent January follow-up were most welcome. Maybe everyone who keeps asking questions has a similar roller coaster experience, but not everyone who has that experience comes to the conclusion that “I” am one of the variables in treatment. I absolutely agree that the power of our interpersonal behavior needs better analysis and understanding.
The concept and term “use of self” which Lezanne used, has been in use since at least 1995, please see my references below. PT has paid little attention to this vital aspect of the therapist’s contribution to treatment, which, I suspect, is why you thought she coined the term. We are the link between the science and the patient. The only aspect of treatment that we can ultimately control is how we “use ourselves”. I became acutely aware of this when I was a clinical instructor and found myself introducing that idea to every single student that came to me.
We can be “… facilitators of change”, as Helen states. Commonly, people who take on that responsibility with people in need of help, spend time seriously reflecting on their own behavior. In school, PT students are rarely made aware of what an important component of treatment they are. I believe that as helping professionals we should acknowledge that it is our responsibility to study ourselves, just as we study the many other modalities of treatment. Then, since nothing works for everybody, each person can decide how to proceed.
Many ways to study our interpersonal behavior already exist. PTs don’t have to reinvent the wheel. For example, the concepts of transference and counter-transference apply to human interaction, not just to psychoanalysis and psychology. We need to have interpersonal behavioral options to choose from, and we need to learn how to choose our most productive option at any given moment. Carol Davis, a PT whose book I reference below, has done an excellent job of presenting these ideas.
Thank you for bringing up this question, it has long frustrated me. It seems so dumb that, except for discrete individuals, our profession has not examined this issue, or perhaps it has already been considered and discarded. It could make our work richer and more productive. It certainly has enriched mine and given me options I didn’t learn about in school.
I took Explain Pain, bought the book for me and my doctor, who loved it, and I am planning to attend your presentation on Feb. 13 in Philadelphia. I am drawn to how you think and the interesting questions you propose. I know you are very busy, but because this is so important to me I would appreciate any sort of response. Thank you, Deborah
Arnd-Caddigan M, Pozzuto R. Use of Self in Relational Clinical Social Work. Clin. Soc. Work J. 2007;36(3):235–243. Available at: http://www.springerlink.com/index/10.1007/s10615-007-0103-7.
Curran, K. M., Seashore, C. N., & Welp MS. Use of Self as an Instrument of Change. Proc. Organ. Dev. Netw. Meet. Seattle, Washingt. 1995:69–70.
Heydt M, Sherman N. Conscious use of self: Tuning the instrument of social work practice with cultural competence. J. Baccalaureate Soc. Work. 2005;10(2). Available at: http://www.mcnellie.com/525/readings/heydtsherman.pdf.
Taylor RR. The Intentional Relationship, Occupational Therapy and Use of Self. Philadelphia: F. A. Davis Company; 2008. Available at: http://www.fadavis.com. ISBN 10: 0-8036-1365-2
Davis CM. Patient Practitioner Interaction, An Experiential Manual for Developing the Art of Health Care. Fifth Edit. Thorofare, New Jersey: SLACK Incorporated; 2011. Available at: slackbooks.com.
Hi Deborah,
Many thanks for the response – looking forward to catching up in Philly. I agree whole heartedly – I think physical therapy, indeed most rehab professions miss or do not want to delve too deeply into the interaction part, after all, if you do it well it exposes self.
I am a bit slow perhaps but in the past I always thought that I was assessing the patient (that is what we were taught and what is still taught) but in reality the patient is assessing me, every little thing about me.
In course curriculum design there is always the “what do we take out to put the new stuff in” question and sometimes a fear of blurring professional boundaries. It took years to get the study of pain as a core subject in our university and there few in the world even now who devote such time to it.
I think our aim should be a core subject broadly called “self” and it should be a part of all rehabilitation courses. I suspect that may take some time.
Thanks for the references too.
David
Thank you for writing on topic of the professional roller coaster. I have experienced much the same in regards to being effective with patients and continually searching for the next effective tool in the tool box. Aside from having a patient that is open and willing to work towards getting better, I have found treatment methods and techniques are more or less effective depending on how I feel about them. Making positive change is most easily accomplished when I am focused, engaged, and determined to make change. Perhaps this is how we utilize “placebo” effectively. I believe it is more than that, as focus and intent seem to be the key variables. Rather than what I say and how I sell it. In fact have never felt like trying to sell anything was ever effective. So staying engaged and interested is the state I (we) need to aspire to. For me this striving for a balanced life and continuing to work on learning the next thing that will make me a little more effective with that particular patient problem.
C. Clarke Tanner PT, MPT, CMPT, ATC, CSCS