
I notice more and more as I read and talk to people and look at the various handouts that practitioners send us at NOI, that we are going through a bastardisation of the Explain Pain work. Dumbed down versions of Explain Pain are all the rage – as if a simple 5 minute video clip, on its own, is enough to alter deeply held pain concepts, or prescriptive treatments that assume pain is a universal experience for all, with a minute on this and two minutes on that. It’s almost a return to the horror days when therapists offered 10 minutes of hotpack and 5 minutes of ultrabullshit. Perhaps worst of all are interventions that include some useful explanations of pain, followed by a “traditional treatment” based on out-dated assumptions that pain starts in the periphery – thus perpetuating the fantasy of pain generators and pain endings in the tissues.
I must be grumpy!
Oooh, I just re-read that first paragraph and I must be quite grouchy at the moment! Practitioners send us their pamphlets, books and handouts with the best of intentions – good on people for at least trying an educational intervention. Please don’t stop.
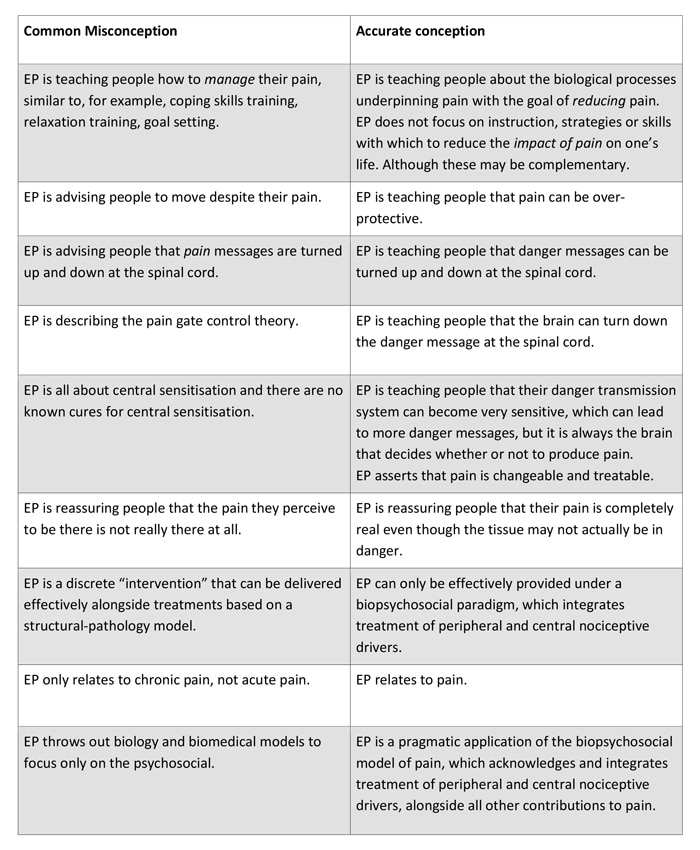
Perhaps the problem is that many clinicians, therapists and practitioners just don’t understand the Explain Pain approach. Misconceptions abound about what Explain Pain is, and we have to take some of the blame for this. Lorimer Moseley and I have tried to summarise these misconceptions and provide accurate conceptions in a recent paper (Moseley and Butler 2015). The table below is an adaptation.
Getting serious about education
Article 26 of the 1948 Universal Declaration of Human Rights states that “everyone has the right to education” thus initiating the Education For All (EFA) movement. Few of us are trained in education but a fundamental difference between life as a clinician and life as an educator is that as an educator with an EFA goal I must adapt, whereas in health, broadly, it is the patient who is required to adapt. Walk through an education faculty and note the different departments and names on doors – gifted, remedial, indigenous, sensory and physical needs etc etc. The educator adapts in a way that addresses individual differences in striving towards the goal of EFA.
And so should we with health education. Quality Explain Pain is tricky as it must be delivered on a framework that indulges changing neuroscience, evidence based multimedia, conceptual change and learning theory, and clinical reasoning. There is no place for short cuts or one size fits all.
“I’m already using Explain Pain.”
When clinicians tell me about how they are using educational strategies, I will often say “tell me about your current curriculum”. This is usually met with surprise, yet the notion of curriculum, while poorly considered in the health domain, should be fundamental to individual and group education. It makes the educator consider issues like content, key learning objectives, appropriate metaphors and similies, tailoring to group or individual, using multimedia, timing, dealing with outliers, understanding the influences of chronic pain on learning, place, associated teaching skills, measurement and reinforcement.
Where next?
While not new, I feel that Explain Pain is at a somewhat perilous stage of its clinical integration. The attempts at simplification that ‘dumb down’ rather than add any value, the misconceptions that abound and continuing outright rejection in some therapy quarters, all threaten to derail this evidenced based intervention. All of this at a time when we are also seeing some positive signs too – Explain Pain making inroads into professions other than its traditional ‘home’ of physiotherapy, clever clinicians the world over truly embracing a biopsychosocial approach and integrating quality pain education with modern thinking about manual and movement based therapies, and a new breed of young researchers that are working as hard on their EP curriculum as the other aspects of robust trial designs.
Overall, this is a call to be careful with Explain Pain – to understand what it is, as well as realise what it isn’t, to acknowledge the skills required to effectively deliver Explain Pain, and develop them where necessary, and finally, to recognise the need to think differently and more broadly, bringing in the rich world of education science and psychology, in the effort to achieve the very worthy goal of pain education for all.
-David Butler

Reblogged this on Neil Wise Physio and commented:
An emphatic David Butler explaining what “Explain Pain” is and is not! The road to an enlightened approach is sometimes derailed by well intentioned short-cuts! Thanks David & NOI
The problem as I see it is the scale of complexity.Before this shift in my thinking I would simply take a case history,examine,treat and give advice.
Now I have to consider the following:-
the symptomatic tissue,the pain matrix,Screening tools -STarT
Back,Orebro,McGill etc,exercise,diet,sleep,genetics,social life,early life experiences and allostatic loading.Their anxiety levels,anger,resilience,illness and injury sensitivity,self efficacy,fear avoidance,catastrophic thinking,depression as well as a quality examination( to help reduce anxiety ,build on self efficacy and reduce catastrophic thinking !).
Now I’m not complaining as I find my practise has become a lot more interesting.However I have found the need to study areas like CBT,acceptance and commitment therapy,mindfulness and problem solving therapy(a simple evidence based approach for manual therapists I believe).
I have travelled down these paths due to the need to have tools beyond a common sense approach to cognitive and maladaptive behaviour.
I feel that we are in a better position as manual therapists to combine approaches than psychotherapists as we can offer an understanding of their bodies(I have also become very interested in embodied cognition).However this is a lifetimes work and it is understandable if the vast majority of practitioners want to stay in their comfort zone.
Plus I admit to still rubbing,stretching,clicking because private paying patients can sometimes get miffed if they have come to se a manual therapist and get a lot of chat.I very often change approach if I feel I’m onto a loser.
Thanks – I really enjoyed this response. I wonder if with all these new skills that you are still simply “taking a case history, examining , treating and giving advice” although now it is really powered up?.
And all those screening tools and questionnaires – maybe we need to question whether they really help, after all with so many of them, who is right? Maybe the time spent filling them out is the time when we should be listening to the wounded story teller and extracting educational targets
Thanks
David
PS -I am all for rubbing and clicking as judicious and educationally lined acts too.
I want to add that as a physiotherapist who is a member of a brand new paediatric chronic pain program, interdisciplinary in nature in a tertiary care centre, all the more reason to have an interdisciplinary approach! I realize this is particularly challenging in the private sector, but the number of components that should be taken into account when doing a true assessment and the number of areas of expertise suggest that multiple clinicians are valuable, no?
I have been introducing EP to the rest of the team… I am counting on it being more incorporated into our developing curriculum and way of thinking. The psychologist is already well on board!
Thanks.
Kathleen
Dave,
Start a clinic. Train some people to your standards. Hire a marketing guy who will promote your clinic Australia-wide. Get results. Let the public themselves do the work for you (via word-of-mouth and social media).
Most Physios really aren’t that smart. Most Physios will tell you (for example) that back pain is caused by “jammed facet joints”, but Joe Public knows that his back plays up when he’s stressed. Most Physios will perform very complex and forceful manoeuvers to “unlock the joint”. Joe Public knows that his back just needs a good rub, but he goes along with the rigmarole….the circus.
Use the public – they are smart. They will spread the message if you get the results. But you have to get the results. Forget about trying to educate “professionals”. You’re whipping a dead horse there. Universities have got a stranglehold on the school leavers. They teach them ultrabullshit because it suits their agenda. It gets ingrained.
EG.
Hey EG,
I have had a clinic all my life! I could spend my entire days responding to chronic pain sufferers’ emails , letters and calls to NOI….and being always aghast at what we do to each other in the name of health.
And yes – I agree that the public has a massive, untapped and often willing mental capacity that we in health reject
David
Right, sorry about that I thought you were full time educator/NOI nowadays. Well…let’s see more videos! They are winners, for sure. How about some really nasty chronic cases or severe acute pain. Need not be the whole treatment – snippets are fine. Show your readers more real life examples.
Theoretical concepts are great. But I’ve often found I have to work long and hard to translate theory into practice. There’s no school where you can practice such things, no mentors who will sit and watch you hone your skills in EP concepts.
Practical examples allow us to see that all-important application, even if it’s just one man’s version of it. The great part about EP is it is very much an art form, so we can impart our own personality. The scope for improvement is enormous and that’s a nice thing for us to remember. “Wow” examples are very motivating. I get that whenever I see a good hypnotist ply his trade.
But it is hard. Infinitely harder than learning a bio-mechanical approach.
[Tim can you remove my name from Dave’s post? Cheers.]
Yo Dave,
You have every right to be grouchy about how EP is being bastardized, watered down, and performed poorly. If you and L are guilty of anything, it is underestimating the sloth of most PT’s when it comes to working, practicing, and researching to develop real skill in the application of techniques. This is just not EP. I had been involved with the McKenzie institute for a long time. To this day, it amazes me how many PTs say that they know how to do the McKenzie technique and demonstrate a poorly performed press-up. When asked how they decided to do the press-up, how to make modifications, etc., they have no idea. “McKenzie is easy- do the press-ups and give them a lumbar roll and book- we learned that in school”. It took me about 8 years of serious study, disciplined-reflective practice, and mentoring to get it right. The vast majority of PT’s seriously underestimate how complicated and difficult good PT is. I have worked hard over the last 8 years to develop the basic knowledge, language/communication skills, and application skills to where I can apply EP well. I had to undergo a fundamental reframing of my view of pain and how that impacts the lives of the individuals and the people around them. I understand how difficult that is for patients because it was very difficult to reprogram my brain to understand the differences between nociception and pain. I also spent a tremendous amount of time looking at the research and taking neuroanatomy courses to update and reframe my understanding of the brain. It was hard work, but I have always thought that my patients deserved no less than that from me.
In the US, at least, I lay much of the blame for this at the feet of PT Education. I left PT education in the 90’s as I saw the homogenization of PT education occurring that created this bland curriculum that focused on the eclectic presentation of material. It made everything simple (details and expert practice were left out) and the schools did not want to offend any specific “school of thought” in the profession. Schools presented a little or just enough of everything. In the process, however, students never learned how to become an expert in something. The inspiration to become and the learning of how to become an “expert or the superior clinician” should be the focus of professional education. To me competency was never enough. MDT, EP, GMI, MFR, Maitland, Mulligan, etc. are just examples that should be used to learn the process and skills required to really master something. Hopefully in time all of these alphabet systems will become passe’ as research and our knowledge base expands and practitioners are forced to become experts in the applications that have more validity.
Dave, you got me fired up. Let me go back to my coffee and enjoy the beautiful morning. In the meantime. I have only two more weeks before I retire.
Thanks for your work, your passion and your witbness. TGD
John – my grouchy old mate!
For once I agree with everything you say! I hope that many people read your response and reflect.
Maybe, when the trout are not biting, you should come out of retirement every now and then?
Thanks for everything
Dave
Having spent the last 20 years trying to do this better, I find that the key to effective education is really deeply understanding the patients beliefs, previous experiences, and understanding before giving any advice, it may take several visits before I feel it is the right time to deliver any sort of education, am also constantly surprised when after delivering what i thought was “effective education” when i ask the patient at the next visit to tell me what they remember that I told them, to be told “you said it was all in my head”.
Hi Rachel,
“You said it was all in my head” still happens to all of us. Please excuse my sales pitch but I think Lorimer and my “Explain Pain Handbook” with the Protectometer and DIMs and SIMs really helps to identify, clarify and grade the “beliefs, experiences and understanding” which set up the educational targets. I am sure you are doing a similar thing anyway.
And there will always be a patient (and I think they are growing in number ) where the response to “you said it was all in my head” can be answered with “well actually yes – it’s right through your body etc etc…. Many therapists are acquiring the skills the skills to follow though with this response .
Thanks
David
Hey David – we all get grumpy when the highly valuable and effective work we are sharing with others is changed – but I take it that this is not the thing bugging you the most – rather, it might be that the education people are providing to people in pain, based on EP, is NOT helping people get better. One of the things I think might be considered is ‘what is the curriculum through which we can effectively train PTs to provide effective pain education?’ Tough question, with a whole lot of words needing clarity, but I bet you, others in NOI, and other colleagues around the world who have been trying to do this have a whole lot of experience in what it takes to learn the information, in what other skills and expertise is required, and how long is required to practice the education, in order for it to effectively shift patient beliefs, attitudes and behaviours. A recent post of yours discussed all the things you thought were necessary to EP effectively – and I take it from that post and this one, that the curriculum to become an effective EP practitioner needs attention.
Hi Neil,
I couldn’t agree more. The research shows that EP is an effective intervention but of course this is research carried out by trained researchers in a research environment. While the training of the researchers could improve (something we are working on now with better curriculum design etc, the practitioners are the critical target.
I do think the often unfamiliar notion of curriculum should be the focus and probably the first question for all to answer is “in this group/person what are the key educational performance indicators, ie the things that must change. (Nociception/pain differences are usually such a performance indicator).
I am not saying it is easy either!
Happy to go into this in depth.
Cheers
David
Hi David, Keep the faith. It works and it works well. Maybe I have the advantage of not being a medico or psyhsio so not full of preconceptions. I’m from the other side, two years as a chronic pain sufferer, gave me the opportunity to research why it hurt. What an interesting odyssy it is. Book list includes all NOI books, Mindfulness , ACT, RFT and Stoic philosophy , Feldenkrais and Hakomi ( yes I get a christmas card from book depository) have been such an eye opener. At 53 I’m of to school to do Mind and Body and Kinesiology . Thank You so much to all at NOI.
PS I live in Adelaide, maybe a coffee one day, so much to tell of my experience with pain.
Hi Dave,
you are so right! There’s a need to expand on good ideas – not dumb them down or paraphrase them as if they were your own.
Sadly I share your pessimism in all of the field of pain education. So few people actually have merits to teach pain science to professionals but courses are flourishing all over the Globe. Why is it that most physios would never take a Maitland-based course from someone who has not actually done any Maitland-training but willingly sit down for days listening to ‘experts’ explaining pain science when these self-established experts don’t have any formal training or academic degrees in pain science?
Don’t get me wrong there’s nothing wrong with sharing others thoughts or delivering a message to colleagues. But don’t pretend it’s original or something unique – just tell it like it is and acknowledge the sources.
Or even better: Rather than competing with each other on delivering similar stuff under various names (or misconceived understandings of the original), maybe it’s time to review the IASP Curriculum for professionals and start adding knowledge to the field? Imagine if everyone was adding knowledge to the field rather than playing copy-cat. How great would that be for our patients!
Reblogged this on videnomsmerter and commented:
Alt for mange mennesker forsøger at slå plat på hvad smerteuddannelse (og smertevidenskab) er.
Det undrer mig, at så få fagpersoner er kritiske overfor hvilken faglig ballast underviserne på de mange ‘smertekurser’ egentligt har. Verdensorganisationen for smerte, IASP, har fx udgivet et curriculum (uddannelsesprogram) for fysioterapeuter, psykologer, sygeplejersker mv. samt et for eksperter (core curriculum). Det ville da ikke være urimeligt at forlange, at dem, der underviser andre i smerter som minimum selv har uddannelsesniveau svarende til deres eget faglige curriculum???
På http://www.smof.dk kan du i løbet af meget kort tid finde en dansk udgave af curriculum for fysioterapi, der giver et bud på emner og omfang af den basisviden fysioterapeuter burde have efter internationale standarder.
Nedenfor er et indlæg fra David Butler, forklarer han hvordan mange mennesker reelt ikke har forstået budskabet i bogen Explain Pain. Det illustrerer min pointe ganske udemærket.
Thanks David – we love hearing those stories and it is a reminder that the process of recovery usually takes time and hard work.
And Morten, thanks – you have got me fired up!. I can’t believe the creative vacuum in our professions and particularly in this area of Explain Pain. I am an avid consumer of the literature, and it seems there are groups out there waiting to see what Lorimer Moseley does next so they can copy or adapt, I read material where I can hear myself speaking, I see images from Explain Pain badly redrawn or just stolen without attribution.
I just want to scream sometimes – THINK and CREATE – the field is massive.
David
I think a big part of the problem with explaining pain is time. We simply do not have enough time to explain the mechanisms and strategies laid out in EP. As a result, people look for a simplified way of doing this, and what they do instead is dumb it down. What I mean by this is they remove the smart pieces of EP and replace parts of complex biopsychosocial explanations with dumb biological, or psychological explanations that are quick, and usually incorrect or very near it. Time is the key I think. It is quick and easy to say, “You have pain because your L5 disc is herniated and we can fix that with surgery.” or “Your L5 disc herniated because you bend forward too much, and we can fix that with extension exercises.” It is much more time consuming to explain pain. As a result physicians continue to perform ineffective interventions for LBP such as surgery, patients stay confused, and PTs continue to abandon things like treatment based classification because they may have to actually do some in depth explanation of why the back actually hurts (because the brain detects sufficient threat, and deems pain necessary to protect the organism), in order to get the patient to buy in, and make treatment effective. The fact is, Mckenzie is quick and easy to explain, the biopsychosocial model is much more time consuming.
Hi Patrick – Yes it can be time consuming — quality evidence based interventions often are. What price for turning the life of a person with chronic pain around?.
I do think as we get better at it, that we can provide the educational intervention faster and more economically. This includes use of groups, use of media, patient homework, therapists getting better at picking up the key educational performance indicators that have to change, distillation of complex neuroscience into metaphor , clinicians having a store of stories etc.
Thanks – don’t give it up!
David
I’m on board with all y’all. I sense “uptake frustration” though. Recall that on the Bell curve distribution of worldwide PTs, Innovators live in a tiny slice at the far right (similar to tiny Andorra). They are the Thinkers & Creators that you envision, aren’t they Dave? Early Adopters occupy a slightly larger space, still in the vast minority (say, the Netherlands?) The huge majority live in the middle (or sadly, the far left) when it comes to uptake of quality treatment regimens. They are the Copiers, who don’t typically innovate or adapt, they just follow. Don’t you think that the first 2 groups have yet to show enough proof in the pudding to convince the majority to vastly alter their practice? ie; there has not yet been a so-called Tipping Point? And that the sea change that is or needs to be occurring will take its own sweet time, and there is only so much that can and is being done (thanks NOI group) to expedite that?
Hey Jeff,
That help somewhat! I think the tipping point in Explain Pain and Graded Motor Imagery will be well after I have carked it (Aussie for passed on!) How do we blow up the pudding and show people what is inside? Its certainly not just research although there are 15 RCTs on Explain pain with all showing similar and useful outcomes. It has to be a cultural change, but (with grumpy hat on), there is too much greed and ignorance out there. Patient and public led change may be the way.
I need to see another game of ice hockey!
Cheers
Dave
What’s your opinion about EP concept in acute pain treatment? Do yo think it’s really usefull as an analgesic tool? Do you have any experience?
I think it would be good idea to break the dualistic “acute” and “chronic” pain. First and foremost it is all pain though the acute/chronic terms are very sticky .
From the hard science world there is some evidence in “acute” pain, and there are RCTs going on now, though most research is on “chronic” pain.
But forget the research and look around – Knowledge has always helped acute pain – its in our face all the time. Things don’t hurt so much when you have knowledge of safety. Earlier this year, my acute chest pain vanished when I was told there is nothing wrong with my heart.
David
Love this article. The more Explain Pain spreads throughout PT, into other professions, and directly towards patient, the better it has to be taught. Such a simple and straightforward table and article helps guide us as learners of Explain Pain to become better educators. Each person will have their own way of using and teaching Explain Pain, but guidelines and intermittent grumpy posts are valuable in keeping the information pure, even if the packaging changes.
Go Cynthia! – I think I will get grumpy more often. Hang in!
David
The stuff on conceptions and misconceptions comes from the tradition of student learning research (aka phenomenography) in higher education. There are two aspects. One is that learners usually come into a course with a lay or common-sense conception of a phenomenon and the second is that they have a set of unconscious assumptions about what it is to learn. If those are about memorising stuff taught in their course, this can just leave their existing misconceptions untouched – and they may well re-emerge as unconscious shapers of practice later on. So a conception of pain framed in terms of a ringing bell or pain gate model will survive the tests for entry into a profession and the graduate will not have shifted their assumptions. In this respect, a quality professional education (and CPD) must engage learners in a critical review and rejection of existing conceptions and require and reward the conscious adoption of more expert and research-informed conceptions – in other words the unlearning is as important as new learning.
Too true, thanks,
And I guess this is a major reason for the emergence of the conceptual change theorists as well as the educational learning theorists. Patients come to us with existing knowledge, often flawed and I think a reason why Explain Pain has been slow to take off, is that conflict it often required to deal with this effectively.
Also, conflict is sometimes needed when dealing with health professionals who are stuck with specificity theory or old versions of gate control theory.
Too many clinicians avoid this conflict. Better to keep the patient coming back forever in their view.
David
This is an important information for all the healthcare providers who treat anyone living with chronic pain. The science of pain is broken down into very accessible language and illustrations and it has brought me an entirely new understanding of how to address the issue.
Ashraf Abdelhamid PT.,PhD.
Great – many thanks Ashraf. You are right – it’s
all health providers.
David
interesting article David but note most of the responses are from physios.
I am a gp with special interest in pain management and 35 years experience
I am also a grumpy old bastard
My thoughts for what they are worth
Why do you describe pain generators as a fallacy ?Targetted treatments in context of a good holistic approach are helpful as all you hands on therapists know
I agree many doctors perform interventional treatments which are expensive ,unhelpful and injudicious but this is not always the case
Poverty is a major issue in managing persistent pain ,often overlooked
It is very hard for these patients to get good biopsychosocial treatment and as therapists we need to lobby strongly for more money to manage this cohort
Complex presentations such as failed back surgery ,opiate dependence,depression, obesity and diabetes (all in one patient)are common in my practice .Unfortunately opiates often impair cognition and make education bloody difficult
5 minute videos and dumbed down handouts are an entry to explain pain not an answer .Chris Hayes of HIPS whose group produced the brain man videos is the first to agree with this For the record his explanation of success in his clinic is that he has great allied health clinicians who spend time talking to patients and are good educators
Norman Doidges latest book How the Brain retrains itself is a really useful addition to the explain pain story
I think you and Lorimer do a great job with your innovative education programs
I also think its time to liase more with the medical side to further improve and enhance the explain pain message
Hi Ken,
Welcome – I love grumpy GPs. But I am really pissed off with your lot at the moment. I have just finished a 2 day Explain Pain seminar in Port Macquarie. Forty people came, which is great for a rural area – multipdisciplinary but NO medicos despite invitations. Doctors don’t want to pay to come to courses. And yet most of the allied health professionals there, on half the income of a GP pay to come along. Most GPs are too cossetted, tight, indulged by drug companies and still many think it is beneath them to learn from a physiotherapist. And increasingly it is becoming clear they are a critical weak link in overall pain treatment.
I agree with much of what you are saying (and Chris Hayes is a diamond in the pain treatment world ) I found Norman Doidge’s first book really useful, but the second book is bugging me though I am not finished yet. He talks about pain generators and pain signals but they do not exist. And too much emphasis on miracles for me. He needs to get off his lofty Psychiatrist perch and just try dealing with someone with a severe stroke, and have them pee in your shoe to realise how bloody hard it is.
I would love to met up and have a grumpy old bastards beer one day.
Cheers
David
G’day again David
Sadly a lot of your comments about my colleagues and our management of pain are true We still cling in a major way to the medical model in managing pain with radiologists ,orthopods pain specialists and many gps absolutely focussed on a “physical cause ” and hence an interventional or prescribed treatment as the answer
In fact I see the medical model as a major perpetuating factor in persistent pain as in bulging discs, “bone on bone” ,back of an 80 year old, wonder your not in a wheelchair,bony spurs and other bullshit
I do quite a lot of talks to various medical and allied health groups and commonly get why should we listen to you ,your only a gp , so its not just physios we don’t listen too!
Have a look at comments in Australian doctor mag from about 8 weeks ago when Lorimer wrote an article on pain as an output phenomenon . They varied from vitriolic to just plain sad!
So, what can be done about it?
You guys have a great message but low penetration in the medical world(is this an international experience as well?)
Seems to me the way the message is delivered has to change
Example, the BIM website some good info but lots of theoretical waffle and pedantic input which is not useful
I get you don’t like pain generators , so what do I call my arthritic right knee which pisses me off and stops me doing stuff?
Happy to meet up (I live on the gold coast but ex Adelaide )and discuss but prefer red wine to beer
Cheers
Ken
THIS! I am an American Physical Therapist, who graduated at the peak of “Biomechanical” theory of pain and “dysfunction” in 1997. Over the past 6 years, I have gradually changed my mindset on pain, which was triggered by my own experience with chronic pain, starting while recovering from bilateral mastectomy, radiation, reconstruction. I began suffering with intractable pain on the cancer side, in chest wall, axilla, lateral rib cage and into scapula. I became the patient, and was steadily declining in my normal recreational activities as well as ability to practice the profession I so loved. I was/am the “manual therapy specialist” and prided myself on my ability to treat the “complex” patients, but due to my own experiences as well as those handful of patients that just didn’t get better, I began searching for other explanations, and that is when I discovered you! I still practice manual therapy, but no longer, but no longer claim that I am changing the tissues themselves or magically unfreezing adhesions 😉 I regularly cite scientific research that refutes any ability to do such things, while also explaining the primary role of the nervous system. But if I have to spend one more visit (and in fact it ends up being multiple visits) undoing the damage done by some ignorant, careless GP, I may just scream and my coworkers will probably have to send me home. Just the other day, I was evaluating a new patient (whom I’m proud to say I did not perform one useless “special test” I learned in PT school), and she literally said “My doctors have me scared to move else I might break something” because of what they reported from my x-rays and MRI’s.” AHHHHHHHHHHHHHHHHHHHHHHHHHHHHHHHHHHHHHHHHHHH!!!!!!!!
There, I had to do it. Anyway, she is a 75 yo active female, with osteoporosis, whose imaging revealed multiple old thoracic compression fractures, along with the usual DDD, spondylosis, facet hypertrophy. She was referred to me for neck pain following a motor vehicle accident, no h/o pain in her back (where all of these scary compression fractures were!), but after these imaging studies, her GP told her he doesn’t know how she is even moving with the damage she has in her back, and she needed to see a surgeon. After reading her imaging studies, I calmly explained to her that the majority of the changes seen in her spine were part of the normal aging process, just as the wrinkles and age spots on her skin were, and that they had no bearing on her pain or function. She is an intelligent, well-read person, so we discussed in more detail how the brain determines what hurts, and how this changes based on threat level, and that the language in her imaging reports, as well as that used by her doctors, have already elevated the threat level, thus making her more apprehensive, etc… She responded quite well, immediately, to this type of education on pain, however, most patients who have been told things like this by their doctors, do not. So, like you said, until there is widespread change in the medical community of doctors, we will always be facing an uphill battle with regards to Pain Science.
David, just a big thank you really. Your book, your work has supported my own discoveries in my practice. Pain free soft tissue mobilisation, coupled with explaintions, matching their tone, accents, empathy. The amazing pictures, in the book. All have aided towards recovery for are long term chronc pain folks, giving them the chance of be able to take charge of their own destiny
Reading the EP book, then hearing Ben Davis, gave me the courage, confidence to share with people we treat, and they do remember what we tell them!!.
But I can really understand your ‘grumpy’……don’t want dilution
Hi Sue,
You say it all – “has supported my own discoveries in my practice.” This what we love to hear!
Many thanks
David
Ken,
I notice David hasn’t had a chance to answer the question about your knee, so I’ll have a crack. Unbidden I know, but I figure it’s a public discussion and you can ignore me if you want.
Your knee hurts because your subconscious perceives a net threat to your system. The brain weighs up all available inputs (including nociceptive inputs from the knee) then decides whether to output pain. That’s EP. How could your situation be different to your patients with back pain?
Hi Dave ,
Ken has some good practical points to consider especially around the demographics . Carr et al have a good article out Time to flip the pain curruliculum which is worth reading and relevant . Heretically perhaps I think there are far more important things than explaining pain ‘properly’ and my attitude/approach has changed over the years. I used to weigh in with the biology explantory models after attending courses but not so much anymore. I feel that understanding pain biology is very useful indeed but very often transferring that information in ways that I was taught not so much for many ‘difficult’ cases. As Ken suggested very often we are dealing with co morbities and pain is one bit of the multisystem chronic health issue . Its all the non measurable /interactive skills that one needs to pay attention to and my own reaction to the emotional displays of suffering . Another seldom raised point is the fact that facing pain and suffering is not a neutral process –it can be a draining and difficult ‘transference’ process which little time is spent considering.
Unless one works in a really good m disciplinary genuinely caring empathic clinic one cannot hope to influence these problems single handededly as the messages are contradictory ie I try to explain pain whilst the medics do the’ pain’ blocks. I think the explain pain skills are important in the far less disabled typical outpatientc clinic populations –the biggest skill is demedicalising and doing much less. I think you might underplay the way explain pain skills are delivered perhaps ie the tone of voice the body language the turn of phrase etc and this needs therapist/medic self awareness. I think all the measurement tools / recording/theapy regimes/paradigms may screw this up sometimes?! I think there is a massive role to look at humanastic approaches in education –we are dealing with displays of suffering where neuroscience in my opinion does not have the answers. The thoughts of Cassels and others offer much food for thought…… http://www.ncbi.nlm.nih.gov/pubmed/7057823
However, we can overcomplicate things massively too so if Ken was a patient and not a GP depending on his lifestyle I would give him an enthusiasitic article by an orthopod on the role of cycling and mild/mod OA and tell him this is definately the way forward and given the results of two TKR this week suggest he literally get on his bike……….. I would find out much more about him after a brief cursory exam of his knee. Its great how physio has evolved and it has a lot to offer the medicalised world we live in …’treatments’ need to be much simpler but the understanding of people/pain behavior needs to be broader overall I feel .
Thanks EG
I understand what explain pain is trying to say(mostly)
My comments relate to more widespread acceptance of the message by doctors
trained in a medical model
Seems to me to be a bit Monty Pythonesque to “out” the phrase pain generators(the words we cannot speak)
Damaged bits of the body are more likely to hurt than bits that aren’t damaged in my experience. Why is this an issue?
Thanks Ken,
“Damaged bits of the body are more likely to hurt than bits that aren’t damaged in my experience”.
My experience too, and it makes sense because tissue damage will tend to trigger nociceptor firing.
“Why is this an issue?”
Maybe us Physios make it an issue because we know that we can’t influence tissue healing or structure. A prolapsed disc or sprained ankle can be protected from further damage, but we cannot otherwise help the disc/ankle to heal. The body does the healing it on its own, at its own rate.
Makes me think… If the body represents some sort of holographic projection of the mind, surely we should be able to alter tissue health via mind processes. I know it sounds ambitious, but so was EP 20 years ago.
cheers
Hey Dave, love the comments but… I think you’re being a tad precious. What with accusing your readership of bastardising, and ultrabullshit etc. I understand it must be galling for you to hear people utilise your branding term of ‘Explain Pain’ interchangeably for their own efforts in Pain Education. I trust that you’re not presuming that your limitedly defined curriculum is the only approach that could be used in providing patients with knowledge about their condition. This might otherwise be known as health education (a fairly well-established concept) or could more generally be termed Pain Education. Perhaps if you were a more open exponent of pain education rather than your own EP course content, and did not use peer reviewed journals as a vehicle for self-promotion, you may take a more kindly view of the efforts of the great number of therapists trying to implement to the best of their abilities Pain Education as part of a more comprehensive pain management approach for their patients. We all love our back slaps, but it is obviously not the most helpful ‘educative’ approach from an ‘educator’ to disabuse your readership of their apparent misapprehensions (otherwise known as ultrabullshit-sic). In this regard, I wonder if you should consider taking some responsibility for misapprehensions which may persist from some of your neural mobilisation courses such as treatments of “stretching nerves, wringing them out” -wringing the bjs out of them 🙂 so as to “improve axoplasmic flow” as the theoretical construct underpinning your management of brachialgic pain or the promotion of contorted body positions to achieve mobilisation of the sympathetic trunk – you gotta think that was a leap of faith??.
In looking at your ever expanding list of promotional material I note that in your “explain pain handbook” you identify yourselves as “the authors who really started the revolution over a decade ago”. Far for me to underplay your significant contributions to pain management, I do think that it is somewhat ungenerous considering the body of works by other researchers in the area pre dating your initial book titled explain pain.
Ooops – I must be cranky too – a wet June and pre winter solstice – I apologise if my comments are too ranty or have resulted in an unintended interpretation. I want to congratulate you on the range of material that you have presented to the clinical community over recent years to assist in pain management. Your inimitable and engaging style in presentations truly maximises the impact of your message. However I would also like to emphasise that curricula vary even between centres of educational excellence and one does not invalidate the other. I am glad that you recognise that pain education is only one component of a much more complex intervention in a chronic health problems such as chronic pain. I do appreciate that in a previous blog you have retreated or found unsatisfactory many interventions which you promoted in the past, however recanting clinical concepts requires redoubled efforts to overcome the seeds of faulty information which have taken root. Best wishes for your upcoming speaking tours. Happy days – the sun is out again 🙂
Hello Michael,
I was waiting for someone to disagree – that was a rant of yours – some bits I can nod and think “well I can see how people think that”, other bits I find offensive. And thanks for the nice bits too. A few comments…
I guess I need to state again that I enjoy it when people take aspects of explain pain and adapt it, use it, make it their own (but do it well) , integrate other forms of health education and I encourage the use of coaching, mindfulness, hypnosis CBT etc. and I help where I can. One key way has been creating the awareness of curriculum. With that basis you can do what you like as long as it answers your objectives. That’s your objective not mine.
But there is a bigger issue at stake here and that is what this blog post is implicitly about. And it is not just about Explain Pain –it’s about any newish and novel interventions. Many clinicians just don’t reason, they only know how to follow (universities can be at fault here) and there is downright dishonesty. We all know that notions of IP are at risk these days,, but even more it is creativity which is at risk. The lack of honest creativity with EP saddens me.
I have already commented on the dumbing down of EP, the mass use of images and text without the courtesy of any attribution. (It only takes a permissions request). Adding insult to injury is that 80,000 copies of Explain Pain have been torrented ie stolen and downloaded for free. Even part of that would be nice, especially as the book funds research back into EP and graded motor imagery. I won’t be bothered again doing the creative multimedia you see in in EP – someone will just flog it. I note you have an EP Handbook – one reason for foldouts and inserts was to stop stealing.
As for your delve into the past and away from the topic. Yes with Maitland, Elvey, Peter Wells, Louis Gifford and many others, we did explore vigorous mobilisation of the nervous system. That was over 30 years ago. That was how we learned, reasoned and evolved to the reasoning and neuroscience based neural mobilisation of today. I have never encouraged stretching or wringing the bejesus. And I have little very little to recant – I wrote a paper for a special booklet on neurodynamics produced by the Australian Physiotherapy Association over 20 years or more ago – the basis of mine was that a positive neurodynamic test in many cases identifies a sensitive movement not a sticky stuck nerve, therefore reason acccordingly. I thought we had all moved on from stretching .
Also – I would be grateful if you could let me know the body of works of others in pain education via neuroscience education that predates Explain Pain. I abhor selective referencing but like to be told if I inadvertently do it.
Thanks for your post Michael. It really made me think. I reckon that I am getting more precious about the material. I think it’s necessary to combat the mediocrity and dishonesty out there.
Cheers
David
Hey Dave, Sorry but please let me know what you found offensive. Happy to chat by pm
You threw out some pretty heavy brickbats and a few bouquets as if to soften them. You gotta expect some to disagree – even if in silence.
In brief: your EP is your IP but your IP is a subset of PE (pain education – Do you agree?). If theft of your IP is your beef then let people know (it would greatly peeve me too) but I got none of that sense being the issue from your blog – only the pesky masses were corrupting the whole area of pain education (undoubtedly some are). I happily reference your source material and even recommend it to providers as an accessible resource to assist them with patient care.
Re: codswallop or (Ultrab) – I agree that there is much out there to rightly disparage whether from intricate pelvic slip combinations or thoracic rings and loops but your comment was not limited and seemed applicable to anything not so endorsed. Consequently my “delve into the past and away from the topic” – it was just to point out that there were some positions that I could not support and many ideas that you promoted which are beasts that shall not die (my brickbat).
“I find it beneficial to treat the cervical spine in tension positions” 1991 pg 233 (what crazy stuff was that! “Do Sliders slide and tensioners tension?” 2007 – an important article but still referencing the mode of action as “milking, pumping…increasing axonal transport”.
Re body of works – pain researchers have disseminated their works as education –this gets integrated as part of clinical practice – just as biomechanical approaches and patho-anatomical explanations – and yes these can be placebo or nocebo – depends on the light in which they are presented. This process of clinical education / explanation has been an integral part of quality care for sometime. This does not denigrate the originality of your own work – but to be fair don’t you think that to say “really started the revolution over a decade ago” is trowelling it on a bit thick – I mean Melzack & Wall – whom you cite, did publish a bit amongst other research teams and IASP – it really is their raison d’etre. – Hoover were big (and many fine products) but they didn’t invent suction.
Cheers
Michael
Hi David,
Thank you too. Because of your generous and quirky teaching of “us” about pain sciences, I have found myself literally having to sit on my hands and stay with the subjective much longer that I might have in the past. From this full disclosure of the “story” comes some very important aspects related to context and a place to provide validation and acceptance of the history and pain experience. These steps are often overlooked in our “time” and “practioner” constrained interactions with patients. It is through this process that I have experienced patients finding renewed HOPE and from that some self ownership of possibility of recovery. The personal context is the place from which the individual application of the skills and language you have offered us to explore with our patients can be applied. It has cracked open my practice and it is very rewarding.
Always thank you!!
Leanne Rath FACP
To EG and David
Can we compromise and accept there are central and peripheral pain drivers?
Ken I’d use different terminology, but only to distinguish the fact that pain can’t happen until all inputs have been weighed in the brain, no matter what is going on.
Take for example a knee with a normal MRI, but clinical signs of an inflamed medial meniscus. The patient has just been through a marriage breakup. His brain will probably output strong pain. If he’s happy about the breakup he might find his symptoms improve or disappear altogether. Importantly, the level of nociception could be identical in both situations.
Clinically, I find it almost impossible to tell how much (if any) nociceptive input is contributing to a symptom of pain. Even symptoms which behave ‘mechanically’ can’t be trusted to have a purely nocicptive origin. Adding to the difficulty is the fact that a lot of the degenerative signs we see on scans are in tissues which have very little or no nerve supply (menisci, discs, articular cartilage).
Regards,
Thanks Leanne,
It’s lovely isn’t it? I think we have been very fortunate to have learned a clinical reasoning based assessment. I have only really clicked in recent years, how good the reasoning based assessment it is to pick up the personal context which then provides the majority of the educational targets for explaining pain. I know it is much harder for practitioners who just follow a more algorithm style of assessment.
Cheers
David
Hey Dave (Hello seems too H.A.L like)- would love to talk off line. I have neural mobilisation 91; the sensitive nervous system; both editions of explain pain and painful Yarns – and appreciated them all – I also did my own little handouts about parts of pain before explain pain but got lazy and because explain pain was more comprehensive – so our stream is probably better of as pm 🙂
I agree that we should acknowledge the sources rather than playing copy-cat. Regarding acknowledging originality credit should be given where credit is due:
I think we are ignoring one of the biggest and most profound contributors to this “revolution” and the perspective in Explain Pain: Louis Gifford. In fact, as I understand it, he actually ran a course in 1999 with Heather Muncey called Explain Pain. When you read his 1998 paper (“Pain, the tissues and the nervous system”) and his essays in Topical Issues in Pain from 1998, 2000 and 2002, I find the ideas and perspective in Explain Pain (2003) permeating through all these pages and yet I see no acknowledgement of his contribution in neither EP nor the EP Handbook besides a small reference to talks about pacing (EP, p114)?
Given the volume of Giffords writings and teaching and his description of his journey here (http://giffordsachesandpains.com/my-pain-journey/), I get the impression that his contribution to the perspective and ideas in Explain Pain has been an unfortunate omission for last 12-15 years. Am I mistaken here?
Hi Adam,
Louis Gifford and I taught together right through the 90s and developed 5 day courses with patients with our best intentions of merging manual therapy, graded exposure and explaining pain. Some of the current interest in pain, at least in physio probably did emerge from our joint endeavours but sadly there is only one of us left. We still talk fondly about those courses and Lorimer Moseley often mentions that a LG/DB course was part of his research topic stimulus. One source of the Explain Pain material was the old “neural tension” courses eg p.200 MOTNS and then we took it a lot further on these 5 day courses. Louis was particularly good at it – a real natural and on reflection, he had a very broad view of pain for the time. You can find my summary of Louis’ professional contributions in a document I wrote supporting his honoured membership of the MACP.
After the Sensitive Nervous System, I saw no need for detailed referencing in my later texts, nor was there a source to reference. Lorimer Moseley did the research work for Explain Pain and this is still continuing, supported by EP sales. The education contributions to EP, later texts and current courses came from my education doctorate, all on a framework of emerging pain sciences with hundreds of contributors. EP is not a heavily cited book – after all it is for patients, but Louis is in there a couple of time. Louis had plenty of opportunities to write about educational therapies in his publications but unfortunately there are no writings on educational therapy to cite, nor am I aware of a course called Explain Pain back in the 90s. My view is, and perhaps Louis would have agreed, back then, nearly 20 years ago, both our attempts at explaining pain were at best primitive. Despite our rigorous post course analysis of the patients over numerous beers, we probably didn’t have that much to write about or anything that a journal would accept.
This is not easy to write, nor am I interested in further contributions on this topic.
But I am really pleased that you have created an awareness of Louis’s contributions to the field.
David