
‘Shin splints’ are a real problem out there – common, painful, activity limiting and often treatment resistant. A bit of research on ‘shin splints’ (or the more recent, awkward, and I am not sure helpful term, ‘medial tibial stress syndrome’) in the medical databases, won’t provide much clarity in aetiology or agreement in treatment and you will find there are probably many different kinds of shin splints. If you Google ‘shin splints’, in-line with the growing trend, you’ll get lots of diagrams with multiple strips of brightly coloured tape applied in complex patterns.
Sometimes you need to be aware of the science, and move on. Move on to what you see in front of you – clinical scientists are often years in front of desk scientists.
Here is a clinical pattern I have seen many times over the last 30 years.
The history
I recently caught up with an old friend while teaching a course in Brisbane, Australia. She is a keen golfer, mid 40s, and had a left tibial fracture 3 years ago – it healed well and she was back to good quality golf within months. Six months ago she began to experience medial tibial pain radiating to the posterior medial malleolus in her left leg during and after golf. She had a medical check up – there was nothing sinister and no complications from the fracture. She also saw a number of therapists who proposed muscle imbalances in the leg, ‘switched off glutes’, trigger points and biomechanical issues in her feet – she had been told that both her feet were ‘flat’. Various therapies had been diligently applied and adhered to, including strengthening, stretching, suctioning, needling – even a bit of ‘core stability’ (perhaps this last one was thrown in as a ‘just in case’).
The end result for my friend was that she was avoiding golf and if she did play, used a cart to minimise the amount of walking. Especially, as she had been warned, on uneven ground.
The examination
I checked her out. There was nothing exceptional in the leg at the time of examination – nothing surprising at all for a 40 year old, active woman who had been fully functional for a number of years post fracture.
However, there was a clear neurodynamic finding which had not been examined in the past. In the slump position, with left ankle dorsiflexion/eversion and knee extension, the tibial area pain was recreated. Releasing knee extension released the tibial symptoms, as did releasing neck flexion. The same test on the right side revealed hamstring tugging and a better range of knee extension. I reasoned these to be relevant findings.
Post examination thoughts
I thought that there were two critical elements in the clinical presentation of the person in front of me. Firstly, and most importantly, an avoidance behaviour based on the (erroneous) fear that playing golf or exercising and experiencing any pain meant that there was further damage occurring and things were getting worse. One comment from my friend went something like ‘If I keep playing golf with my muscles all out of balance, the trigger points will come back and I’ll just make it worse’. Secondly, there was the relevant neurodynamic finding. If I was trying to be a bit smart, I might suggest that a third clinical element was a positive feedback loop between these first two, with the fear-based ‘though viruses’ helping to drive a sensitive nervous system which in turn provided erroneous evidence for the thought viruses to be maintained.
The treatment
We treated it. First I suggested not calling it ‘shin splints’ – this metaphorical diagnosis suggests that the problem needs support or outside help – aching shin, even just sore shin is better.
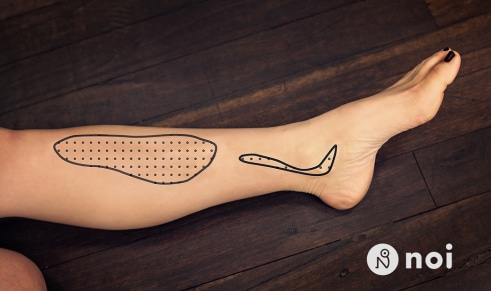
Secondly we moved her nervous system around a bit with the idea of restoring its sliding and gliding function and maybe flossing and flushing out some areas that had been a bit ‘sticky’ for some time.
We have recreated the assessment and treatment in the video below:
[youtube=http://www.youtube.com/watch?v=fkSJKXF2IQ4&w=1280&h=720]
Thirdly, we chatted. I suggested that there may be a bit of an increased ache for a day or so post stretching as this sometimes happens but not to worry about it ‘It’s your body adjusting to the treatment’. I suggested that the problem now was a ‘bit of nerve and soft tissue irritation, it sometimes happens, even a few years after an injury as the brain holds memories of serious injuries and can react over time* – almost trying to heal it again so it puts a bit of useful swelling there which can irritate things. It gets a bit compounded when treatments don’t work or make sense and you start to worry – worry can make things more sensitive too. But this is all good – it will go. Go back to golf – there’s nothing that can be damaged – play 18 holes – a few aches and pains are fine and normal, continue the post game gin and tonic ‘
She played 18 holes of golf 2 days later – no problems. It’s now 3 weeks later, and with much golf and regular stretching there are no reported problems.
My thinking
Not all ‘shin splints’ are the same of course – some acute presentations may be serious medical emergencies** and should be treated as such. But my example is a common and repeated scenario and I believe that this problem is not often treated in this way.
This is not intended to be some crowing about a ‘miracle’ – there was no miracle cure, no quick-fix, no tricks, no secret technique performed by magical hands. There was just some basic clinical reasoning powered up by a modern, neuroimmune understanding of how pain works – or at least the best understanding available to us right now.
The kind of pattern reported above is common and will usually ease with the simple principles showed in the video. If I had to have a go at the pathology, I would suggest some tibial nerve irritation, perhaps even a minor compartment syndrome in the posterior compartment which houses the tibial nerve. How simple it would be to suggest that the nerve and its connective tissue sheath were sticky, perhaps with limited oxygenation, some local immune inspired inflammation perhaps also related to slightly altered anatomy post fracture. But more than that – I suggest that the person’s perception of the problem has also added to the sensitivity both locally and in neuroimmune territory representing the meaning and the function of the leg.
I rang my friend today and asked how she was going – ‘I am doing fine. Golf is no problem at all. It’s good to know I couldn’t hurt this paying golf and its good to have some stretches that I know are getting at it’.
Sometimes our game can be deceptively simple?
David Butler,
*We are talking here about a temporal brain glial response – microglia and astrocytes have a danger surveillance function which may last for many years. If activated they may encourage responses in other systems such as the endocrine and sympathetic systems leading to swelling and increased local sensitivity.
**If you ever see or experience lower leg pain that commences suddenly, is associated with rapid and significant swelling of the lower leg, changes in blood flow, tingling and or loss of sensation don’t hesitate, seek appropriate medical assistance immediately.

Pro at work.
Dave, I’d really be keen to see more case studies on video because there’s so much to absorb. Now you say there was no magic, but there were certainly some good positive suggestions thrown in:
1) “Can you feel how it goes instantly?” (this sentence has now been internalized and may well re-emerge later when she performs the exercise at home).
2) “Great, you’re in control” (sense of control reduces anxiety).
3) “Feel the pull, enjoy it” (don’t resist pain, move into it without fear).
4) “Can’t hurt anything there” (more anxiety reduction).
5) “There’s something you can do after to make things really settle” (Compare with say: “this exercise *should* help you”, or worse “this exercise *might* help you”. There’s just no question… it will help).
And the voice is very non-threatening in tone.
Given all this, I can’t help thinking if your friend would have had just as good an outcome without the nerve exercises.
EG.
Just to clarify my last sentence… no nerve exercises but still incorporating all the excellent therapeutic alliance and suggestion stuff. Could it still have worked?
Sometimes I like to just do interferential (IFT) on its own… nothing else. I do this because I know that IFT has no long term effect and so it gives me a good idea about how effective my rapport/suggestion work is. I had an elderly lady this week with a sore knee and she couldn’t walk too well. So I did 3 treatments of just IFT on its own. Sounds insane doesn’t it?! But I sit and chat with her while the machine is on (she talks, I listen) and LOTS of things are going on in that time. LOTS! She’s fine now.
I’m at the point of thinking it’s quite possible to just give everyone 10 minutes of IFT and still get excellent results. But I’ve got some more experiments to do and plenty of skills to master yet.
EG.
Hi Cam,
I am really open to the idea that the “nerve exercise” may not have been needed and that the critical elements included the examination and the “you can’t damage yourself” story. Maybe deep massage may have had a similar effect? In this case it is about reasoning, selecting an appropriate intervention and basing the narrative around it. In another clinical situation the intervention could be around weak and tight muscles or electrotherapy.
Cheers and thanks
David
YO Dave,
What are you doing with such droll clothes!!!! I loved the orange shirts and electric green ties. Are you getting old?
By the way, great video. Videos are great, but people need to know that there is much more here than meets the eye. You make it look simple, as all great clinicians do. Clinicians need to take “the courses”, be mentored, and study. There is a lot of work that went into to making that treatment look simple, straight forward, and valuable. In fact it is if you understand all of the big and little clinical wisdom facts that went into deciding what to do and how to explain it. There is a tremendous amount of “devil in the details” here that should not but anyone off but spur them to learn more.
As I get older, I really appreciate watching masters, no matter what the discipline, at work. I applaud not only your technique, but all of the years of mastery that went into that performance. Thank you for sharing that.
JohnB
Many thanks John,
As you know, my attempts to contribute to the profession have also included enhancing professional fashion consciousness. I have always enjoyed being polychromatic.! You should have seen the socks and undies that I had on during that clip!. And you are so right – there is a lot of work that goes into making something look simple in the clinic. But digressing back to colour – it is also a small part of the clinical magic. I have always held the notion that a patient (and student) must come back curious. And if “what will he be wearing next time?” is part of that then so be it.!
Very best wishes
David
I really did enjoy the endorphin rush of the typo on the original post! A great example of a belly laugh to reduce pain perception. It was really funny! A great example of the holistic approach.
That being said, I agree that all those positive suggestions help make the treatment more effective.
As always, I enjoy reading your thought provoking posts David.
This really makes me wonder about the clinical reasoning and that goes on to support the interventions that you mentioned that your friend had trialed.
From a bio-mechanics perspective, these are, I assume, probably rationalized in terms of reducing torsion or forces that may have detrimental effects on tissues, presumably contributing to inflammation and peripheral sensitization. In the ‘current medial tibial stress syndrome’, this ‘sort of makes sense’, but I VERY MUCH WONDER what those same interventions may have achieved within a different language context with the therapists being mindful of what their patient was cognizant of during and after Rx sessions.
I would propose that reassurance to move, reduction of cognitive error and thought virus taking home and rumination (by way of asking the patient to paraphrase their understanding of the therapist educational/cognitive input), in combination with some ‘distracting’ (yet perhaps biomechanically helpful and mechanically risk mitigating) exercise homework might have resulted in quite a different outcome – possibly without needing peripheral nerve mobes to desensitise…?
I also wonder if (cat amongst pigeons, not being a current disciple of and still a sceptic of) kinesio taping may play a role in non-threatening, distractional, non-noxious sensory cortex stimulation, reducing threat value, improving confidence to move, all with the polychromatic, possibly individualised and favourite happy healing colour scheme of the patient…???
Andrew
Hi Andrew, That’s all fair enough. A lot of people have got better in the past from therapies that did not even contemplate neural structures. In this situation, trying to be uncorrupt in my clinical reasoning as I contemplated the periphery/health of tissues area , I found more support for peripheral neuropathic contributions than anything else. I can conceive of some scar in connective tissues, a local immune response, a little bit of acicidy, bit of oxygen starved tissue, some sluggish gelling axoplasm etc – all needing a bit of a wring out and flush (how scientific is that? !!).
Coloured kinesiotape??. Its just like when you make an appointment to see the doctor – your pain eases – you have done something about it, added some safety – same as sticking a bit of tape on – add a bit of colour and you have done something special. Lets hope its not all the therapists do!.
I remember taping up football teams ankles in my youth. I am sure my saying “I will put a heel lock in as well” helped more than the sticky stuff.
David
“I remember taping up football teams ankles in my youth. I am sure my saying “I will put a heel lock in as well” helped more than the sticky stuff.” Yep, did a version of same myself and certainly thought the same!
Don’t know if it was ironic or cosmic, but I had a professional ballet dancer last week with similar symptomatology and history (long term “shin splints” problem that morphed into intermittent medial shin pain with distinct avoidance behaviors). I had a feeling that none of her previous clinicians looked at the neurophysiology of her case, so I proceeded (literally with your work in hand) to assess the LQ nerves. Lo and behold, clear signs of tibial, sural and femoral nerve involvement. She had more going on than just her lower leg issue, but that was the chief complaint. I look forward to reporting how this weekend’s performance went for her, which was a big thing as she is casted in a principal role. Thank you, NOI!
Bob
Thanks Bob – let us know. This also links into Frédéric’s question below.
David
really enjoyed this and the reasoning —what i particularly homed in (apart from lack of polynesian/dame edna inspired fashion) was this *We are talking here about a temporal brain glial response – microglia and astrocytes have a danger surveillance function which may last for many years. If activated they may encourage responses in other systems such as the endocrine and sympathetic systems leading to swelling and increased local sensitivity.
can you send links or expand on this?? —so relevant clinically esp to the stressed /confused person with lots of explanations ….I have had complex pts who have been labelled as all sorts of obscure Rh conditons and when you hear the narrative that led up to their bodily dysfunction simple measures like reducing loadbearing /education/graded exposure +- minus analgesics have really helped reverse the situation ….
ian
Hi Ian,
The notion of microglia and astrocytes as surveillance cells on the look out for danger to the representation they are associated with, plus their ability to remain activated, experienced or alert over time helps us understand a lot of clinical scenarios.
A good read on the experimental data is Austin PJ & Moalem-Taylor 2010 J Neuroimmunology 229:26-50 – here the data showing local and remote glial responses months after an injury is detailed. An older classic article by Banati R ( Neuroreport 2001, 12: 349-3442) provides evidence of brain glial activation years after peripheral nerve injury. In one case (amputation), brain glia was still active 23 years after. Any by the way, while you are feeling glially – Yirmiya and Goshen’s Normal Cousins lecture – Immune Modulation of Learning, Memory, Neural plasticity and Neurogenesis (Brain, Behaviour and Immunity (2011) 25: 181-213 is a great review .
A person holding the language and image that their shin splints are “torn muscle attachments” or “periosteum pulled away from the bone” has created something dangerous for glial cells to respond to, essentially resulting in an alteration of immune balance (see Austin and Moalem-Taylor for discussion on immune balance). And as you suggest Ian , confusion, and stress and multiple labels adds to the danger. It all help us understand the problem that always comes back.
And even just asking someone “how are you” rather than the “how is that torn muscle” seems to be a biologically better place to start.
David
Yo Dave,
I am very pleased to learn that you have not lost your keen fashion sense. the profession needs more of that. Please keep the undies underwear’s, my nervous system isn’t ready for that. Great work. TGD
You are not the only person who has suggested that John!
that should be undies under wraps!!!!!
Hi David, I enjoyed your blogpost very much, as obviously, my cognitive biases are along the same lines as yours! Although I too find that shin splints patient have altered tibial nerve neurodynamic I often also find some small hypoesthesia on the skin overlying the painful area on the picture. Wouldn’t that be a cutaneus spahenous nerve territory? How to reconcile this finding and the abnormal tibial nerve neurodynamics?
These and other findings across different condition often have me wondering on the meaning of altered neurodynamic findings. Are the altered findings suggestive there is an issue with the nerve tested per se? Or rather, is the finding simply suggestive there is an increased sensitivity of the nerve secondary to peripheral sensibilisation secondary to inflammation in a neurologicaly related msk tissue?
In other words, is the increased nerve sensitivity related to the nerve itself or rather to a parent tissue? Could it be both? (rather likely I would say).
Hi Frédéric,
I would probably reconcile such saphenous changes by the likelihood of multilevel changes in lumbar DRGs and cord, set up by an original nerve issue – perhaps tibial in the posterior compartment . Other possibilities could include excessive deep tissue massage of the saphenous nerve!
I think you have nicely answered the last question yourself. My feeling is that it is rare that the test suggests a singular issue with the nerve tested per se. The moment a nerve is injured remote glial and neural changes occur. Sticky nerves needing a bit of a wriggle and a “wring out” occur of course but much more, I think neurodynamic tests expose specific sensitive movement constructed by peripheral and central responses and pathophysiologies rather than a sensitive nerve. I like the term “parent issue”
David
I was thinking today how the word ‘Physiotherapy’ gives the wrong impression about how the body-mind works. It gives the wrong impression to students and the client population.
Isn’t it time we changed the degree course and called it something new? I propose: ‘Psycho-somatics’. The body is still clearly represented, but the emphasis has definitely changed to reflect new science. Even if Psychosomatics was a degree course for the treatment of chronic pain only, that would be a start. Not a weekend course. Teaching this stuff as a weekend course puts it alongside Rok taping certificate courses.
I feel confident this sort of education will appear formally somewhere in the world soon. How can it not with the ground swell of new information appearing? Uni of SA could be the leader.
EG.
Ah Cam – things change ever so slowly!!!. But it MUST happen. Most OT courses are still psychologically based with minimal neuroscience. Very few PT courses include more than a few hours pain science or the pain stuff goes with electrotherapy. Pain is till almost absent in medical courses. The University of South Australia, to their credit took on semester long (180 hours effort) courses in clinical pain sciences a decade ago but I am not aware of any other institution doing it. (And of course pain is just the default term for the other perturbed brain outputs which are taught in such a course.
Not sure about the term “psychosomatics”. And while on the topic I would love a better word than the mouthful that is biopsychosocial.
David
Neuro-somatic therapy? Neuromatrix therapy? It’s time…
Instead of Biopsychosocial… what about holistic?!! Hehe.
Maybe a cute acronym like PAEP – pain as emergence phenomenon. It brings the listeners attention to the model, and the model can change. Therefore we don’t get locked in to something obsolete.
EG.
Hey EG
It’s absolutely time. But i do fear that as some sections of the therapy world (rightly and appropriately) enthusiastically embrace pain science, the most important people – the patients, can get left behind. I agree that the term physiotherapy (even more explicit in other parts of the world with “Physical Therapy”) sets up an expectation in regards to “what” is going to be treated and “how” – i.e., the physical body (tissues) treated with some physical agent. The failure of most of these physical agents to do anything much at all is evident in the literature – and of course, why would they work given that pain is so much more complex and emergent than the models that these agents are based on?
But, the world at large is still stuck with notions of pain endings, pain fibres and pain pathways and there is still so much work to do to change this. I think if we get too far out in front of the people in pain (I’ve recently seen a PT blogger suggest that he is no longer going to ‘treat pain’ – i could see his point, but i think this would be very confusing for patients). My sense is that the change first has to happen within the various professions and their various labels – and it can. Moseley showed years ago that patients could understand pain science, even though their therapists thought that they couldn’t – or at least underestimated their ability to do so.
The challenge, I think, is to morph the current professions into modern approaches that can take all the good stuff of old (touching, stretching, mobilising, strengthening etc etc) and place them within a ‘holistic’ framework that does not attribute them any ‘magical’ powers and that focuses on education and placing the control in the patients hands.
Once we’re there, we could probably call it anything we like!
(getting off my soapbox)
Thanks EG – always thought provoking.
Tim
Dear NOI family and friends,
I’ve followed this post with great interest, fascinating. All that I can add is that up until 25 years ago I regularly examined diagnosed and treated individuals with “Shin splints”. Since joining NOI and applying their knowledge and experiences i have yet to see one true case!!!!!!!!!
However a true case can be a medical emergency therefore, through solid clinical reasoning I always set out to prove myself wrong.
For me this largely applies to the whole range of peripheral pathologies………..
Beautiful demonstration David, the master at work x
DB
On location
you seen this for some rehab solutions ?! http://www.theguardian.com/technology/2014/nov/06/mouse-chair-office-workers-move
Thanks Ian – time will tell here!
David
Reblogged this on Team PT and commented:
Flushing and Flossing – Interesting read.
I love the simplicity and complexity of our bodies. It is why I do what I do.