Our colleague and friend, Dr Hayley Leake, discusses pelvic pain in women, its prevalence, and research findings from the Pelvic Pain Impact Questionnaire (PPIQ).
When the spotlight hits the stage, back and neck pain seem to always be standing front and centre, while pelvic pain and friends slink quietly in the corner. So it’s surprising when you find out that the prevalence of pelvic pain in women is just as shockingly high as other pain disorders.
‘Up to 1 in 4 women have persistent pelvic pain, and almost every woman has experienced pain during menstruation’.
Now, it’s not just that it hurts, and we would like the hurting to stop. It’s how that hurting affects life. The hidden effect that pelvic pain has on work, social activities, relationships and intimacy for starters. This is not easy information to capture, and until now, there was no quick screening tool to gather this specific, and potentially delicate data. Luckily there are some researchers with their eye set on finding these solutions.
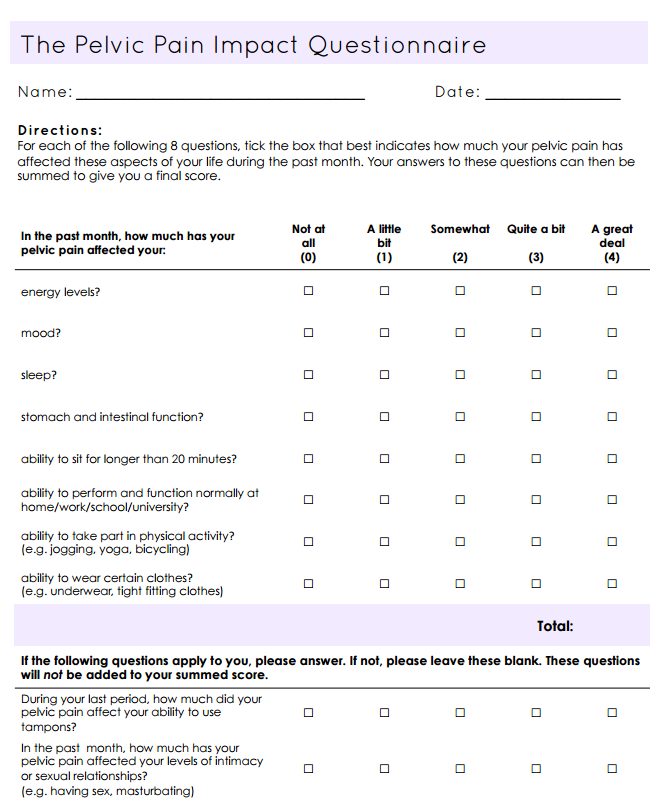
The Pelvic Pain Impact Questionnaire (PPIQ)
Chalmers et al. (2017) have produced and tested the Pelvic Pain Impact Questionnaire (PPIQ) in this article. The questionnaire aims to provide an individualised glimpse into the life impact of pelvic pain. Importantly it takes into account not just the clinician’s, but also the patient’s perspective on what constitutes quality of life.
To figure out the impact of pelvic pain on life Chalmers et al. conducted an eDelphi study. 389 women were asked 52 statements and here are the top 5 concerns (for the full list of the top 25 see the appendix):
1. Levels of intimacy or sexual relationships (e.g. having sex, masturbating)
2. Stomach and intestinal symptoms (e.g. abdominal pain, discomfort, nausea)
3. Mood changes (including feelings of anxiety, depression, anger, sadness, frustration)
4. Using tampons
5. Sitting for longer than 20 minutes
Through three rounds of eDelphi testing, they determined 10 aspects of life most impactful for women with pelvic pain. These 10 aspects were converted to a Likert scale to create the final Pelvic Pain Impact Questionnaire. Our confidence in this measure is boosted as before its release it was rigorously put through a Rasch analysis that showed strong psychometric properties and additionally good reliability results.
How do you use it?
It’s pretty simple really. The person with pelvic pain fills it out (it should only take 5 mins). There are eight questions that get scored 0-4, for a total of 32. Questions 9 and 10 are ‘only if applicable’ and so are excluded from the tallied score.
How would we use it clinically?
Obviously these questions can be difficult for some people to talk about, so providing someone with quiet reflection time to consider their answers and prepare to discuss them, is surely a good thing. Their answers can then be used to guide further subjective questioning to get a deeper understanding of the psycho-social impact of their pain. And when you feel that your clinician is taking an interest in what you think is a priority, that surely must be a SIM.
What are your thoughts. Can you see yourself using this clinically? Would you be comfortable to fill this out for your therapist?
– Hayley Leake
Research Fellow, Allied Health & Human Performance, University of South Australia


We do not get many referrals for pelvic pain but the few that we have seen do seem to be more entrenched in the biomedical model. The psychologist working with us is getting a number of referrals for pelvic pain. I think that Psychologists with good pain education skills have the right training and approach to be able to ask questions that we as physios might have difficulty with. I can see a real opportunity for this questionnaire to be used in this setting.
Its great to have a pelvic pain specific questionnaire – thank you. Do you have any data on what score means what? Or do we just see a reduction of the score as the clinical outcome? I will start using the PPIQ and see how it assists our understanding of our patients experience and if actually changes alongside our current measures. With thanks, AJ
Hey Angela,
It does seem like a helpful resource. My understanding is that the score can be used to track changes within the same patient, rather than extrapolate to other patients groups. So yes, I imagine changing scores reflect clinical changes.
Hope it fits well into your practice,
Hayley
Thanks Hayley. What is the MCID?
Hey Angela,
The MCID is the Minimally Clinically Important Difference – https://en.wikipedia.org/wiki/Minimal_clinically_important_difference
“the smallest change in a treatment outcome that a patient would identify as important”
A great tool, which I will certainly use in my practice herewith. Thanks for sharing, Hayley
You write that the journal article is open access, but when I try to get the pdf, it asks for the OVID login or similar. Have I misunderstood something? Thanks for any help in accessing the full text article!
Hey Sarah,
Ahh you are right! My mistake, writing has been amended. The article is in fact behind a log-in, however luckily the appendix is open to access which gives us some good information.
Hayley
Could we see something like this for male pelvic pain?!
Good idea!! We currently use the Male NIH Chronic Prostatits Symptom Score. Do you have another one you use?
I also use the NIH symptoms score, but as the name suggests it is symptom focused and misses many of the factors that can contribute to a pain experience. In addition I also use the PCS, GAD7, PSEQ along with a general intake form (diet, meds, pain location scores (more specific than the NIH form) and a revised version of the IPQ which can be found here – http://www.thepelvicpainclinic.co.uk/wp-content/uploads/2016/12/Pelvic-Pain-Perception-Questionnaire-1.pdf
Thank you for that questionnaire 🙂
We have many CPPS Patients and I’m looking for more questionnaires and scores. Are there any others you recommend?
Greetings from Cologne, Germany.
These are the ones I use in my practice at the moment. I have found these to be the most beneficial.
Have you come across the UPOINTS system? http://www.upointmd.com