This is one of those useful links to bookmark and share with clients at appropriate times. From The Sydney Morning Herald:
The article also has a nice personal story woven in that patients may also relate to
New lease on life
…Her first surgeon booked her in for arthroscopic knee surgery, but it had to be postponed because of a cancer diagnosis in the family. She never went ahead with it and says it’s one of the best decisions she’s ever made.
“I got more opinions and the third surgeon referred me to a rheumatologist who said I should first consider making lifestyle changes, like losing weight and doing knee-focused exercises, and the pain went down from nine out of 10 to three out of 10,”
“I’ve been doing various different activities because we have a large garden and I haven’t thought about arthritis pain until this conversation,” she continued.
“I’m not entirely free of pain, but there are some days when I have absolutely no pain, and it’s fantastic.”
Bookmark it, Pin it, save it, or, print it and slip it in a drawer – a handy little bit of ‘educational ammunition’ to add to your collection.

I am pleased that Australian Rheumatology Association, the peak body in Australian rheumatology, has made these recommendations. But when will the Australian Physiotherapy Association issue advice to patients experiencing musculoskeletal pain that the practice of “dry needling” of phantom “myofascial trigger points” is not only illogical and unscientific, but also a complete waste of their time and money, as well as being potentially harmful?
Thanks John. The best advice, it would seem, is don’t hold your breath. I found the APA’s response to last year’s kerfuffle over the federal government’s announcement that it was removing pilates from private health coverage, highly instructive.
From the horse’s mouth:
“The APA released a media statement last month supporting the government’s announcement of a reform package for the private health insurance (PHI) sector… It is important to note that the APA agrees with the broad intent of the government’s PHI reform package—that funding needs to be focused on treatment where there is a sound evidence base showing benefit.
However, members should not be unduly concerned about the removal of Pilates from the list of rebateable natural therapies. Any physiotherapist delivering a one-on-one or group consultation on any patient(s), whether it be classed as Pilates or something else, is unaffected by the PHI reform package.
The reform package measures have been set with the understanding that there is a clear difference between physiotherapist-instructed Pilates programs and those used by other practitioners. As a result, physiotherapists utilising Pilates methods in their patient treatment plans will not be affected by these changes.”
It seems that according to the APA, when their members deliver modalities, something magical happens that negates any nuisance “evidence”.
My best
Tim
(if i was being cynical, i might, just might, slightly raise an eyebrow at page after page of advertisements for dry needling and pilates courses in APA publications…)
Tim, your comment “something magical happens” aligns dry needling with homeopathy. The reality of the resemblance is argued in this article: http://www.fmperplex.com/2018/01/26/dry-needling-for-musculoskeletal-pain-the-new-homeopathy/
Tim,
There is evidence that Pilates is beneficial for patients as highlighted by this recent systematic review https://www.ncbi.nlm.nih.gov/pubmed/29332746
Is it the only way to get good patient outcomes, perhaps not, it appears that most forms of exercise are beneficial to patients. Does something ‘magical’ occur in Pilates that other exercise does not offer, probably not, but it has a good social status and anything that encourages people to get off the couch and get moving has to be positive.
The APA should be campaigning with the Government and relative private health bodies to encourage more exercise with subsidies. Who better than to be prescribing and facilitating exercise than physiotherapists
Paul
Hi John,
You have probably produced some literature on this but what is it about “myofascial trigger points” that you disagree with? Is it that a muscle can be a source of pain? That somatic referred pain exists? That pushing on similar points on different peoples body can cause pain and pain radiation?
Those having a heart attack often report pain into their jaw and down the arm, wouldn’t this be somatic referred pain? If somebody reports pain down the lateral aspect of their lower limb, couldn’t it be plausible that the gluteus/TFL trigger point is the origins of their pain? Would be great to get your thoughts
Paul, trigger points have never been shown to be sites of nociception (ie tissue damage). The entire construct was erected on conjecture and its proponents made two fundamental epistemological errors. We pointed all this out in 1994 but our paper was largely ignored. The rest is history.
John, not to start a debate but showing a site is causing nociception is nigh impossible as we do not have the technology to assess for nociception. At this stage the best we can do is inject local aneasthetic into this area however this may work for a variety of reasons and not necessarily from reducing tissue nociception. On a side note tissue does not have to be damaged to cause nociception, as is the case with Delayed Onset Muscle Soreness.
I think it is highly plausible that muscle can be a source of pain and that as we are all humans that biomechnically work similar, we all may get muscle pain from similar sites (these sites may be determined as triggers points)
Paul, the MPS/TrP debate is now over. Perhaps this article will convince you: https://blog.apsoc.org.au/2018/01/08/behold-the-mighty-trigger-point/
John, have read the article. My follow up questions are:
– Can muscle be a source of nociception and hence possible cause of pain?
– if yes, then can this pain be felt in referred areas?
Perhaps the definition of “trigger point” needs to change to “focal area of muscle pain”
Yes, muscle can indeed be a source of local and referred pain, as can all other deep tissues that are innervated. But the MPS/TrP theorists have assumed this to be the case whenever they encounter the clinical phenomena you describe. In other words they have bypassed the process of scientific inquiry and led their followers down a road that ends in a broken bridge. We warned them about this matter in 1994. They have much to answer for.
I think I see what you’re saying, MPS/TrP theorists believe that whenever the encounter what is deemed a taut band of muscle this is therefore the source of a patients symptoms and needs to be treated when in fact these “taut bands” may be innocent
Paul, the MPS/TrP theorists are guilty of passing off conjecture as established knowledge. In so doing, they seduced innumerable clinicians into believing and acting upon their scientifically flawed explanatory model. Undoing the damage they have caused has been no easy task.
Yes I agree, MTrP has been over diagnosed and treated unnecessarily. However this shouldn’t be discount that muscle can cause pain, whether manual therapy is necessary though is a different question. I also think if we are going to question the efficacy of dry needling then we also must question massage as they both are said to work via the same mechanism, temporary effects on the nervous system
Hi,
Not sure how this has descended into a TrP debate….
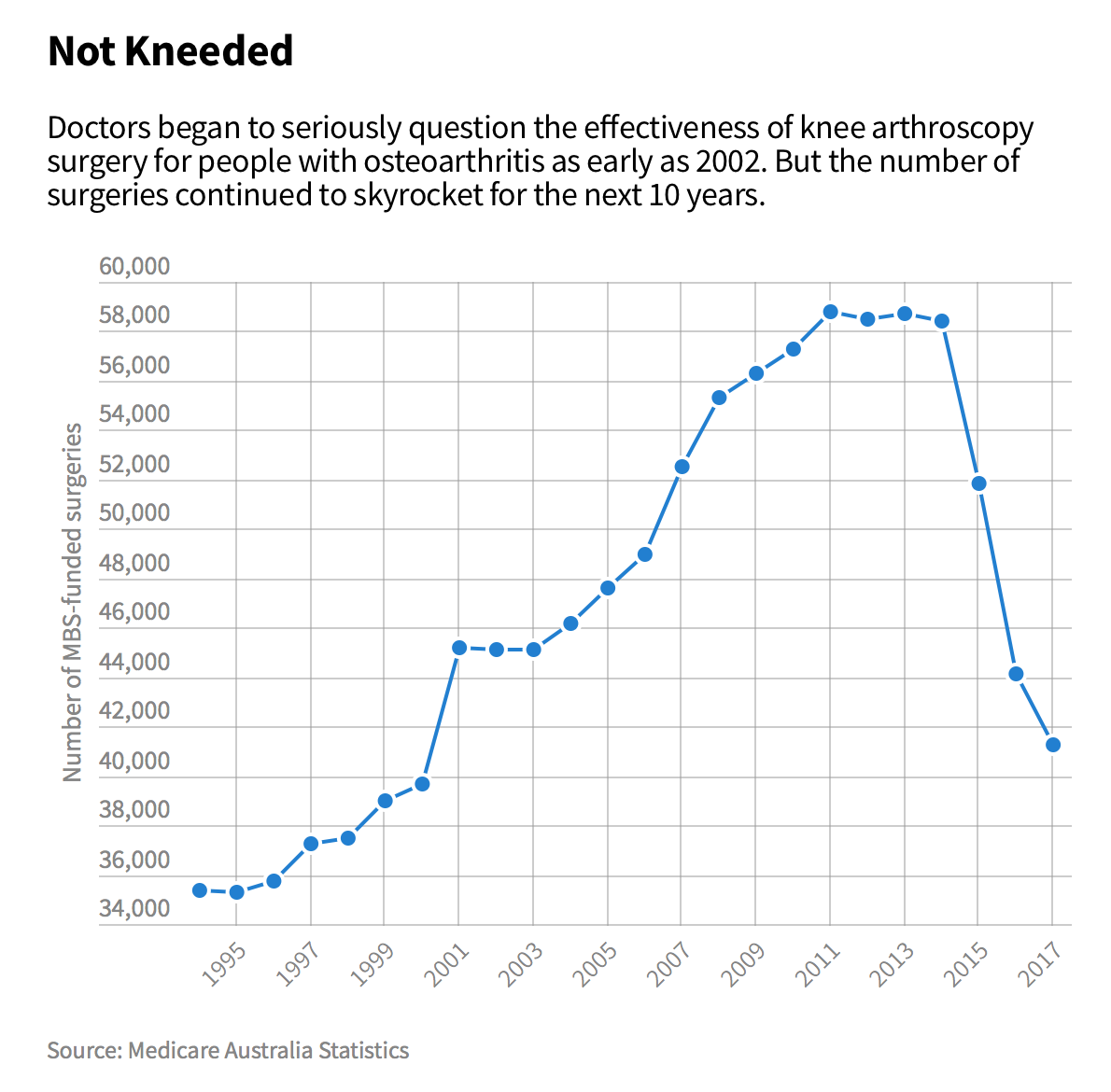
Alas, I am always curious about these graphs and what exactly they are plotting. There have been numerous examples from overseas of similarly graphed trends in the surgical management of degenerative knee conditions, all greatly influenced by data source. eg. arthroscopy with lavage/debridement as was historically done for OA has showed significant reduction in the past decade plus but arthroscopy with APM (differently coded) has drastically increased in the same time frame.
Anyone aware of the Australian data – does this include all comers?
Cheers