There are obvious motor changes that pose a problem when treating stroke patients – very limited, or at times, no active active function of a limb. Graded Motor Imagery (GMI) can sneak under the radar of these physical difficulties, as all of component steps of GMI can be performed without needing to actively move the limb. So should we be using this feasible, inexpensive treatment in the clinic?
In the past we have seen research showing the benefits of GMI for CRPS, chronic pain, and phantom limb pain. We have also seen the components of GMI being used separately in stroke patients – explicit motor imagery, a few times, and mirror therapy, many times. But we have previously learnt that the specific sequential manner in which GMI is provided seems to matter.
“The order of GMI components seems to be important, which is consistent with its proposed mechanism” (Bowering et al. 2013)
Naturally, the next step is to bring the components of GMI together to see if they provide benefit to patients post stroke. Polli et al. (2017) have started this process.
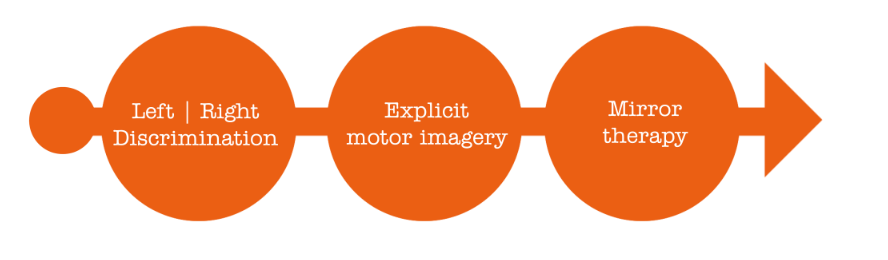
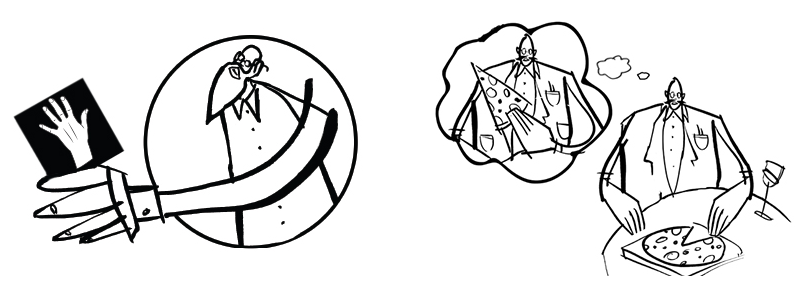
An explanation of how to teach GMI has been well documented in any of the above studies, or also in this fabulous blog. We even created a whole website and wrote a book to walk you through it. Essentially GMI is thought to reflect graded activation of cortical networks and follows a series of implicit motor imagery (left/right judgements), explicit motor imagery (imagined movements) and mirror therapy. It is also thought that GMI acts to reduce cortical disinhibition, also known as smudging (check out this clip).
How did they provide GMI?
- Time: 1 hour session, 5 days a week for 4 weeks of treatment: total 20 sessions.
- Inclusion criteria: first ever ischemic or haemorrhagic stroke; aged 18-75 years; absence of apraxia or sever aphasia.
- Control group (n=14): 2 hours of individually tailored motor rehabilitation per day.
- Experimental group (n=14): 2 hours of individually tailored motor rehabilitation per day, with 1 hour of that time being allocated to GMI.
- Primary outcome measures: Two functional assessments of upper limb
- How: The paper provides thorough details of the GMI intervention – it’s open access, check it out!
What happened?
- 10 out of the 14 post-stroke patients receiving GMI treatment showed important differences in upper limb function, compared to 4 out of the 14 in the control group – perhaps the first step to show the potential benefit that GMI can have on motor function
- Answered some statistical questions to power a future RCT – watch this space
- Questioned if stroke patients have different baseline values for left/right discrimination – hopefully results from this study will gives us some answers, check it out!
– Hayley Leake

Adelaide, 26-28 May EP + GMI
Wollongong, 14-16 July EP + GMI
Darwin, 4-6 August EP + GMI
Brisbane, 25-27 August EP + GMI
Newcastle, 8-10 September EP + GMI

comments