Guest writer, Emily Moore, continues her blog on working with non-verbal children in pain: Working with children in pain can be a challenging and disheartening experience. On top of this, what if the child is unable to verbally tell you about their pain? And what if they only have a small list of predetermined words/pictures to describe all of their pain experiences? In part 1 of this blog, we explored the challenges that children with complex communication needs (CCN) face when trying to tell others about their pain. I also introduced you to Marco – a fictional boy whose story is based on an amalgamation of patients I’ve seen. Part 2 of this blog covers the potential stigma of pain thresholds in non-verbal kids, and discusses self-report versus proxy-report in our pain assessments.
Let’s continue with one of Marco’s many stories.
Part 2 of 2: Reporting your pain, should not be a pain
As I look down at Marco’s augmentative and alternative communication (AAC) device (part 1 has an intro to these), I take a moment to consider the options before me. It is not surprising that I quickly become disheartened. Then freeze. Do I ask Marco to try and type/write his answers? No – he is way too upset for that. After a deep breath, I ask, “Marco, can you show me what you told your mum?”
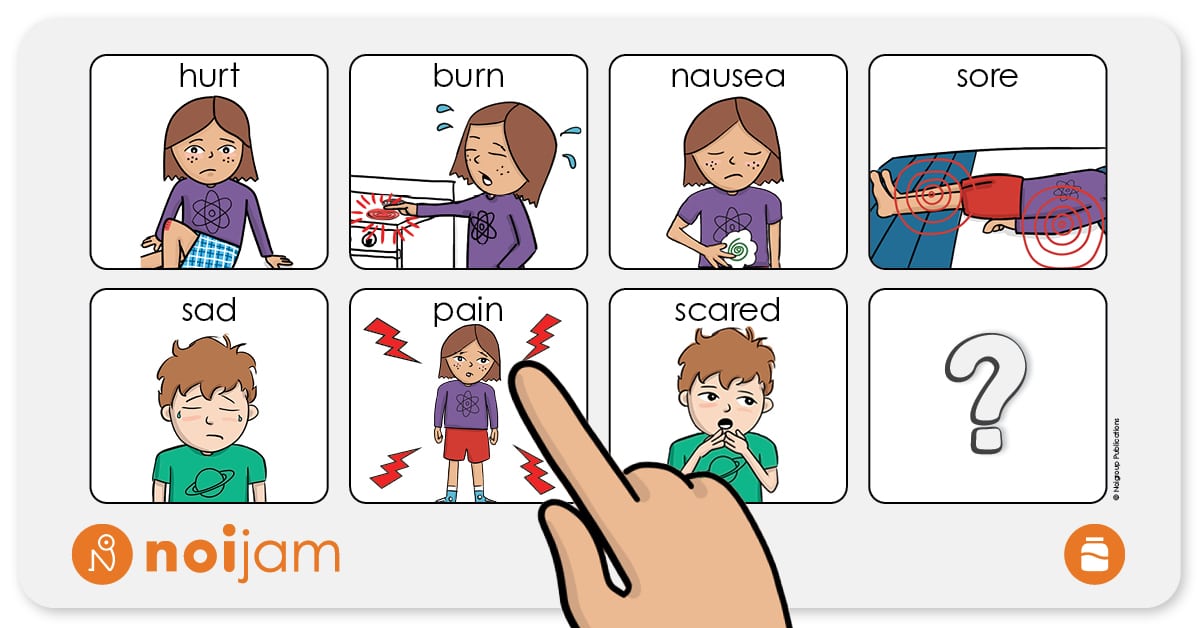
Marco responds:
I reply, “Thank you, I am here to try and help. Where is the pain, Marco?”
After a moment, Marco shuffles in his seat and then points to his new red wheelchair. Marco begins to become more upset. I try again.
“Marco, where on your body is the pain?”
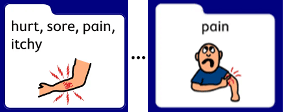
Marco:
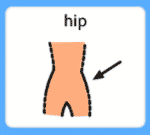
With a smile, I respond, “Good job, Marco. Okay, can I please have a look at your hips?”
There were no obvious injuries or skin changes to his hips. I turn to his mother, and begin asking her about the recent holiday: When did he start selecting the pain option? Did anything happen?
She recounts their recent holiday and adds, “…but he barely ever has pain. I was told he must have a high pain threshold – so, something must be really wrong”.
Marco yells and starts to hit the back of the wheelchair. Out of curiosity, I start inspecting the chair for any potential sources of his pain – any loose screws, pointy or jagged edges.
I pause, what was that? I unzip the cushion and find four small seashells.
In the end, Marco’s older brother had been hiding the shells in the cushion during their recent holiday. The shells were not sharp, rigid, or pointy – pretty, yes – but no jagged edges were found. But the sensation was just enough, that maybe over time, Marco’s brain began to consider these shells a threat.
Mystery solved! Right?
Let me tell you, this was just one of Marco’s pain stories. Most children reporting pain do not have shells hidden somewhere on their seats. How can I even guarantee that it was the shells in the first place?
Let’s explore a few aspects in this story.
Two shockingly common misconceptions with serious consequences
Misconception #1: If you don’t tell us, then it doesn’t exist
In Marco’s story, his mother mentioned that he had a high pain threshold. Have you ever heard this in your clinic? In 2020, the International Association for the Study of Pain (IASP) updated their definition of pain. In this definition, they noted that:
“verbal description is only one of several behaviors to express pain; inability to communicate does not negate the possibility that a human … experiences pain” (IASP 2020).
Why is this emphasised in the updated definition? Because there was a time in recent history when a clinical definition of pain was that:
“Pain is whatever the experiencing person says it is, existing whenever he/she says it does” (McCaffery, 1968).
According to this definition, if someone does not self-report their pain, then their pain simply does not exist! This may have played a part in the misconception that children with CCN and/or intellectual disabilities have higher pain thresholds or are indifferent to pain.
Have you ever heard anyone say:
- ‘Oh, she never mentioned she was in pain, so that must not be the reason.’
- ‘He has a higher pain threshold compared to his siblings.’
- ‘They did not say they were in pain, so they must have a really high pain threshold!’
But how do we know this? What if they simply do not have the means to tell you about their pain?
To this day, it has been speculated that children/people with CCN can have undiagnosed, undertreated and dismissed pain experiences; largely because they do not have the opportunity to self-report their pain to others (Booker & Haedtke, 2016; Johnson, 2021; McGuire et al., 2016; McKinnon et al., 2020; Stevens, 2021). Living with pain that they do not have the words to explain.
It can be hard to imagine a child suffering with pain, just because they struggle to tell you what is going on. Especially when the pain can have a huge impact on a child’s ability to participate in school, their quality of sleep, and can lead to feelings of hopelessness and defeat (Ostojic et al., 2022).
Yet, over time, children with cerebral palsy (CP) have reported that they can grow accustomed to the pain (Ostojic et al., 2022) and think that the pain is ‘normal’ (Hägglund et al., 2020). Eventually, children may stop trying to report their pain altogether.
Misconception #2: You must choose either self-report or proxy-report
In the scenario I have been using, I asked Marco’s mother various questions about his pain. This is ‘proxy reporting’. Looking back, you can see that Marco was trying to tell me what was bothering him from the beginning, but I misinterpreted his attempt at communication as an act of frustration.
‘Self-report’ is considered the gold standard for pain assessment. Yet, proxy reporting can be a good starting point for clinicians to investigate why a child may be in pain. A parent and child often create a language of their own. A parent can help translate a certain behaviour, gesture, or sound for clinicians. For this reason alone, proxy reports have an important part to play in the identification and management of pain in children. Proxy reporting, however, should be used in collaboration with self-report. It doesn’t have to be one OR the other!
Currently, due to many reasons discussed so far, proxy and behavioural methods of pain assessment can often be the only methods used. But a child’s behaviours can still be misinterpreted, even by the most well-meaning of people. For example, a child may be interpreted to have ‘behaviours of concern’ at school, because they may often yell and hit at teachers who try to help with toileting. Their behaviours may be misinterpreted as a dislike to having their clothes touched, instead of long-term frustration that the sling used to assist toileting is uncomfortable or painful.
What if we could give these kids a better opportunity to self-report their pain?
Where to from here?
There is so much to explore here. My PhD is starting to investigate how we can help children with CCN self-report their pain. Please, reach out if you have any experiences or advice to share.
In the meantime, if a child uses an AAC device, have a look to see what pain reporting options are available to them. Could the child be in pain, but they just do not have the words to tell you?
Want to talk more about how pain science education might work for non-verbal patients? I would love to hear from you! Please send me an email (Emily.moore@mymail.unisa.edu.au) or reach out via Linkedin or Twitter. I would love to hear your feedback and potential ideas for the future!
– Emily Moore
BPsych (Hons), BPT (Hons)
PhD Candidate
IIMPACT in Health | Body in Mind (BiM) Research Group
University of South Australia | Kaurna Country
Email: emily.moore@mymail.unisa.edu.au
Emily has two honours degrees – in Psychology and in Physiotherapy – and works in the paediatric sector as a clinical educator for the University of South Australia. She has led and presented two research projects which focused on educational concepts that will guide future material on Complex Regional Pain Syndrome. She now focuses on her PhD, which seeks to investigate pain-related vocabulary for children with and without cerebral palsy and complex communication needs; with the aim to guide the development of more effective communication options for children to self-report their pain.
Want more?
Feature image adapted from Zoe and Zak’s Pain Hacks, Book 3: Zoe and Zak’s Brainy Adventure! © Joshua W. Pate, Noigroup Publications (In press 2022)
References
Booker, S. Q., & Haedtke, C. (2016). Assessing pain in nonverbal older adults. Nursing, 46(5), 66–69. https://doi.org/10.1097/01.NURSE.0000480619.08039.50
Hägglund, G., Burman-Rimstedt, A., Czuba, T., & Alriksson-Schmidt, A. I. (2020). Self-versus Proxy-Reported Pain in Children with Cerebral Palsy: A Population-Based Registry Study of 3783 Children. Journal of Primary Care & Community Health, 11, 215013272091152. https://doi.org/10.1177/2150132720911523
IASP. (2020). IASP Announces Revised Definition of Pain. International Association for the Study of Pain (IASP). https://www.iasp-pain.org/publications/iasp-news/iasp-announces-revised-definition-of-pain/
Johnson, E. (2021). Supporting Communication Vulnerable Children to Communicate Their Pain. In V. Yashasvi Waisundara, I. Banjari, & J. Balkić (Eds.), Pain Management—Practices, Novel Therapies and Bioactives. IntechOpen. https://doi.org/10.5772/intechopen.93588
McCaffery, M. (1968). Nursing practice theories related to cognition, bodily pain, and man-environment interactions. University of California at Los Angeles Students’ Store.
Booker, S. Q., & Haedtke, C. (2016). Assessing pain in nonverbal older adults. Nursing, 46(5), 66–69. https://doi.org/10.1097/01.NURSE.0000480619.08039.50
Hägglund, G., Burman-Rimstedt, A., Czuba, T., & Alriksson-Schmidt, A. I. (2020). Self-versus Proxy-Reported Pain in Children with Cerebral Palsy: A Population-Based Registry Study of 3783 Children. Journal of Primary Care & Community Health, 11, 215013272091152. https://doi.org/10.1177/2150132720911523
IASP. (2020). IASP Announces Revised Definition of Pain. International Association for the Study of Pain (IASP). https://www.iasp-pain.org/publications/iasp-news/iasp-announces-revised-definition-of-pain/
Johnson, E. (2021). Supporting Communication Vulnerable Children to Communicate Their Pain. In V. Yashasvi Waisundara, I. Banjari, & J. Balkić (Eds.), Pain Management—Practices, Novel Therapies and Bioactives. IntechOpen. https://doi.org/10.5772/intechopen.93588
McCaffery, M. (1968). Nursing practice theories related to cognition, bodily pain, and man-environment interactions.University of California at Los Angeles Students’ Store.
McGuire, D. B., Kaiser, K. S., Haisfield-Wolfe, M. E., & Iyamu, F. (2016). Pain Assessment in Noncommunicative Adult Palliative Care Patients. Nursing Clinics of North America, 51(3), 397–431. https://doi.org/10.1016/j.cnur.2016.05.009
McKinnon, C. T., Morgan, P. E., Antolovich, G. C., Clancy, C. H., Fahey, M. C., & Harvey, A. R. (2020). Pain in children with dyskinetic and mixed dyskinetic/spastic cerebral palsy. Developmental Medicine & Child Neurology, 62(11), 1294–1301. https://doi.org/10.1111/dmcn.14615
Ostojic, K., Sharp, N. L., Paget, S. P., & Morrow, A. M. (2022). Lived experiences of pain in children and young people with cerebral palsy. Developmental Medicine & Child Neurology, 64(3), 364–371. https://doi.org/10.1111/dmcn.15061
Stevens, B. (2021). Revisions to the IASP definition of pain—What does this mean for children? Paediatric and Neonatal Pain, 3(3), 101–105. https://doi.org/10.1002/pne2.12047

So great to read this Emily – so very glad to see such a superb bunch of truly respectful and genuinely caring people researching and educating us about pain – the noijam/noigroup mob!
As an adult who’s suffered – invisibly, and mostly silently (“stoically” – ‘shutting up’ was regularly reinforced, in all sorts of ways, when I was young) – from the tyrannies of severe, and, in recent decades, constant and relentless, pain, I am relieved and heartened to read what you’ve written.
A few bits in particular stood out: “Living with pain that they do not have the words to explain.”
And “… can lead to feelings of hopelessness and defeat.”
And, the biggest one: “Eventually, children may stop trying to report their pain altogether.”
All so familiar to me, and currently rather desperately important, as I’ve just got the message loud and clear that my current GP is unable to listen/take what I do say seriously (- sadly, an all too familiar experience, which certainly does ‘shut me down’ – or ‘up’ as the case may be!)
So grateful for your excellent work, and ability to speak about it so clearly!!!
To you, and the entire crew, my warmest and most grateful thanks and ongoing appreciation.
Every best wish,
May McLeod