Our website noigroup.com is getting one very big overhaul. In fact, we’re rubbing it out and starting again. We can’t wait to show you the brand new website in a few months. With the old website being put out to pasture, we want to make sure that the years of collected content don’t get lost, so we will be re-posting some classic old NOI notes to ensure that they have a new digital home. It’s been an interesting process reading back over material from over a decade ago – where have our ideas changed, where have they stayed the same, and so on.
We had a great response to our last NOInote flashback concerning David Butler’s perennial patient Fred. This week we are firing up the time machine and heading back to December 2010 with a look at language and some key conceptual shifts. Many people – patients and therapists both – have made these conceptual shifts, but we think there are many out there who are still yet to get there. It might be useful to reflect on where you stand, and where your colleagues are too on the key conceptual pressure points.
Discs don’t hurt!
More and more people are catching onto the therapeutic neuroscience ‘movement’ in the last few years and it seems that the key conceptual changes required for effective change are becoming somewhat clearer. Perhaps the most powerful is that tissue injury does not equal pain, stated provocatively here as ‘discs don’t hurt’. Most, if not all readers probably know that, and many may integrate the information into clinical behaviours.
The genitals, love and discs
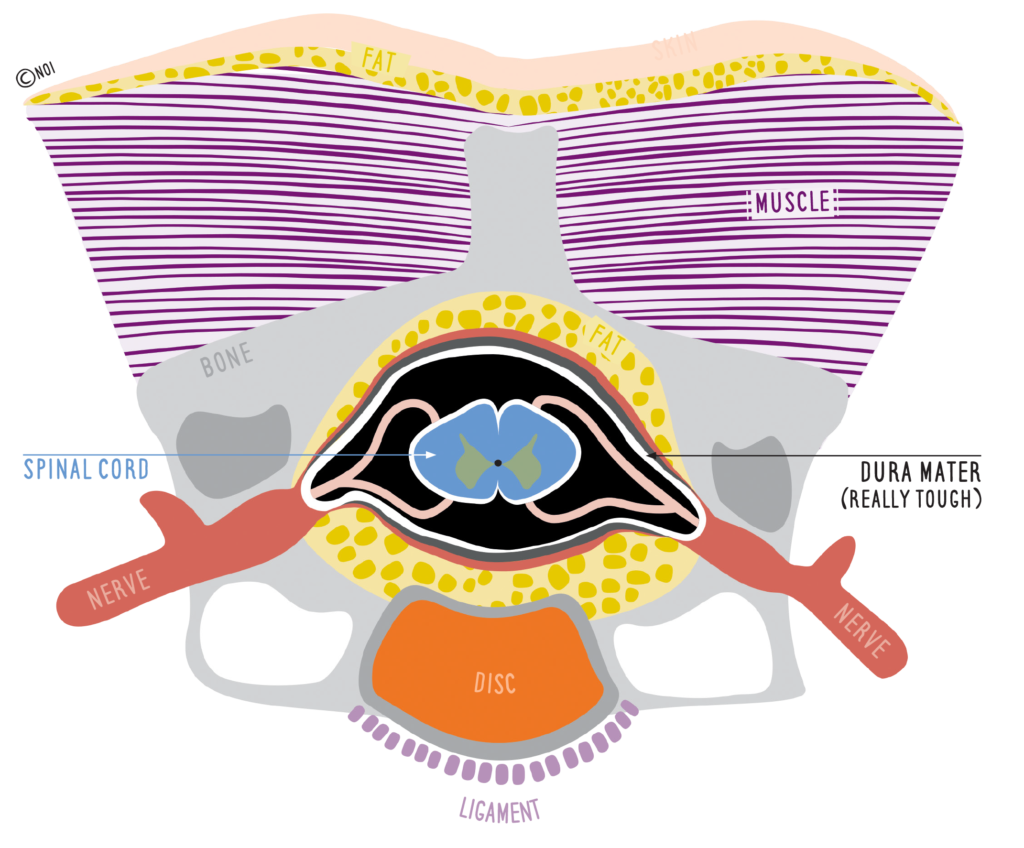
We all (clinicians, patients and the public) say it – “muscle pain, disc pain, joint pain” – all potent wording of a structure attached to a brain response. Yet, it is worth pausing a moment – discs never hurt… all that discs and the products they may release can do is send volleys of impulses into the central nervous system which, depending on whatever else the CNS is constructing, may be a part of a pain schema or neurosignature. You see, if you believe a disc can hurt then there should be a direct link from the disc to your mouth. Or along the same lines, you should believe that genital stimulation can create love.
Conceptual change points
Concepts are the basis of knowledge. Over the last year we at NOI have discussed and argued the key conceptual changes that are usually necessary to help a person in chronic pain or stress and they come down to a small number including:
– pain is an output of the nervous system not an input
– pain is one of many coping outputs of the nervous system
– new knowledge of plasticity gives us hope and novel strategy
– knowledge of pain and movement are effective pain liberators
– the nervous system moves and slides as it conducts
Practicalities
PS: The LAFT
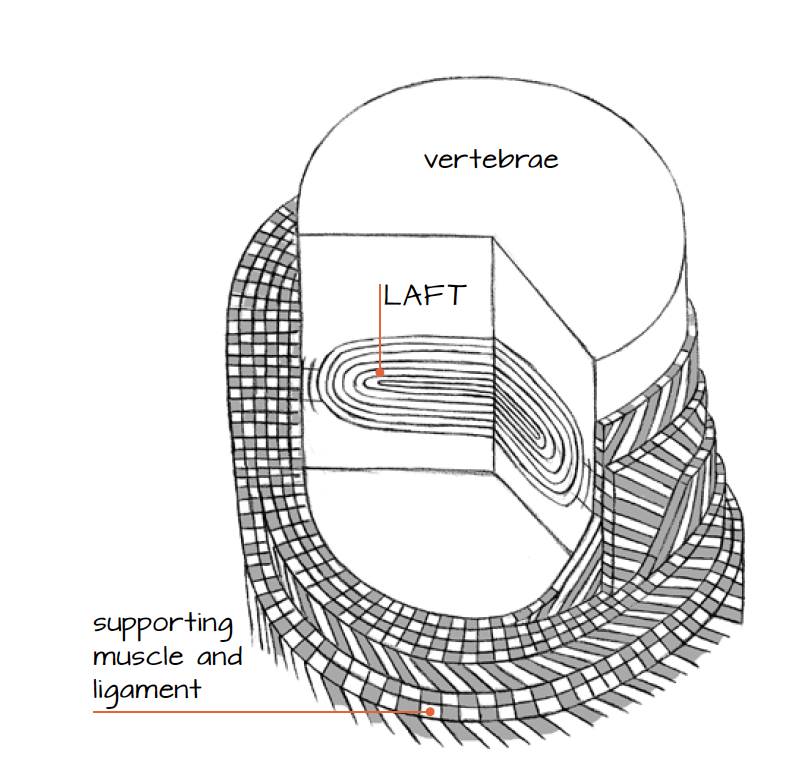
In Explain Pain, Lorimer and I tried to change the name of disc to LAFT – ‘the Living Adaptable Force Transducer’ in an attempt to take away the ‘slip out’ image of a disc. I must admit failure – though occasionally a befuddled student will call and say, “no one understands anything about LAFTS”. I often nod.


Loved reading this today – I had a meeting with 3 GPs yesterday about the Pain & Injury Workshops I run and the overwhelming message was that their persistent pain MSK patients are being let down by a system which has no time to put these messages and diagnoses in context for them – sends them out with a prescription and confusion and no opportunity to explore their fears/myths/anxieties about what the diagnosis means to them. They’d rather send their patients on a Workshop with me than to the multidisciplinary pain clinics 50 miles away…get in the Pain Revolution!!!
Hi. I was introduced to the new concepts around pain about 8 months ago and it has had such a positive impact on my life. Unfortunately this information is not available to my Aunty.
My Aunty, 73, within a two year period has gone from living independently (in a village) in Wagga to being bedridden in a nursing home in Sydney. She has a brain tumor but this is a meningioma (?). There is very little evidence that her symptoms actually are caused by the tumour. What appears to have affected her the most is her belief system and the way information was given to her. She appears to have stopped even trying to walk from the moment she was told she had a tumour. She has given up. She experiences incredible pain, far more than is believed by medicos and most staff. I imagine a lot of pain is simply from not moving her body. Yes, there are other health issues but it’s heartbreaking to see this woman who could have so much better quality of life but won’t get the education or physical therapy required, largely as it would cost too much but also these concepts need to be so much more widely spread to all the medical professionals. Most people have accepted that she cannot improve. She is so miserable. There must be so many people in nursing homes suffering in similar ways and it makes me so sad.
I’m one of the seemingly few lucky ones. Thank you.
Lesley-Anne Sapsford