“What do you mean ‘nerve’, it’s a muscle… mate”
The notion of curriculum has become central to nearly everything we do with Explain Pain – in our courses, as we collaborate with researchers, and as we look towards our next publications and products. Creating a curriculum is what separates correctly done Explain Pain from the ad-hoc ‘education’ that can occur in clinical settings (and sometime research settings too) that is often more about knowledge shows or paying lip service to ‘education’ or notions of biopsychosocialism.
Take a situation where a person has had a bit of hamstring and anterolateral leg pain for 2 months. They report no back pain and their leg pain increases on a longer stride. There are no neurological findings. They think it’s “muscular, probably with a few trigger points – I get those in my neck and shoulders all the time”. From your assessment you recognise it as ‘L5’ish nerve root irritation’ and you want to try and make the whole neuroimmune system (in the region – and beyond!) a bit healthier with some manual/neurodynamic therapy, novel input, homuncular refreshment, exercise, and of course, education.
Explaining this situation can be a bit tricky. Tricky because the person has come with preconceived knowledge that has stood the test of time – for at least two months (but probably years), and tricky because you the educator are aware of the power of peripheralism, biomedical thinking, and the impact that your colleagues have had on society’s understanding of pain and injury.
The need for a curriculum
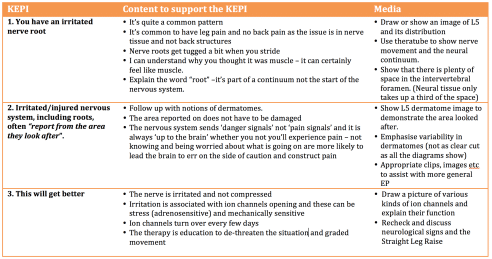
As with any educational intervention, we should have a curriculum, based on what we determine the key educational performance indicators (KEPIs) are, i.e. the bits of knowledge they really need to ‘get’. There is no need to write it down of course, but a curriculum can be a nice statement of what is going on in your mind at the time. This particular scenario should be quite easy – there is plenty of evidence to support your alternative view of neuropathic pain.
Below is a simple ‘mini-curriculum’ breakdown of what is going on in my head (click to see a larger image).
Make a plan, but keep thinking and reasoning
Depending on the individual, I’d want to cover each of these three KEPI’s in a single session, but I’d also be mindful that for some it might be too much. As educators, we need to be ready to adapt – adapt the message, adapt the delivery style and adapt the timing and so on – this becomes a bit of a didactic dance as we adjust continually to the responses of the patient, making sure that we have them on board as we mentally check off each KEPI.
Along the way you can easily add some further evidence based teaching strategies that are quick and easy, and really power up the message – ask the person to explain their understanding back to you, contrast the new information with the old ideas, provide evidence against the old conceptualisation and provide further evidence for the new ideas, use metaphor, analogy and story, get them to draw or copy a quick picture, or ask how they might explain the session to their family when they get home.
At follow up sessions, these KEPI’s provide quick reassessment points – is there anything I need to cover again, have they ‘got it’, are they keen to know more – do I need to go deeper on one or all of them? A curriculum designed and used in this manner isn’t just another document to be filed away with other scraps of paper, but rather a framework that ensures that you are delivering quality Explain Pain, an assessment and reassessment (of both you and the patient) tool, and a clinical map that guides you and gets you back on track if you wander off. Think about a patient that you might be seeing at the moment and intending to provide Explain Pain to – what’s your curriculum?
– David Butler

Nice one David,
Your comment of getting the patient on side is the tough part of education. Out of context it sounds bad but my comment of ” Get an attitude bitch” to the patient the other day sealed the pact between us. She was definitely on side from there on in, Finding a delivery root is the
challenge….
DB on location
😎😎😎
Great post David. I am currently struggling with developing a curriculum of dose specific EP for a few patients in crps. It seems that they both have already transitioned their identity to that of Crps. They are also both readers and have read a lot about crps and essentially chalk a motor their symptoms up to that despite me trying to take an EP avenue to teach them neuroscience. It’s getting sort of defeating. Maybe I am expecting thoughts, beliefs, and sensitization to change faster than I should.. I have had each of them read EP and ask questions of me. I have utilized graded motor imagery with mirror training, desensitization training, and relaxation training via diaphragmatic breathing. I have also tried emailing lorimer to reach out and try to get advice but have not heard back. Can you give a “wet behind the ears” EP clinician like myself some advice with managing CRPS? Thanks mate
Hi Steve,
I think you have quite dry ears!
A few broad thoughts. Of course there are many “kinds’ of CRPS and a curriculum has to be individualised.
Perhaps the Explain Pain Handbook which was always written with CRPS in mind may be more appropriate at this stage. An advantage of it is that it exposes the education targets, many of which the patient (and therapist) may not have been aware are contributing to their pain state.
But here is my ultimate aim…. To be able to say something like this to someone with CRPS, say of the foot – “ wow, look at that foot, you are obviously a very powerful person. You have really turned on some great protective and healing systems and you have done it for a long time…but you may have overdone it a bit. ”
That of course requires clinical skills to unearth why protective systems such as motor, immune endocrine, sympathetic, cognitive and inflammatory are turned on and edgy and then technique (usually educative and graded activity) to deal with them. But to have someone implicitly get the statement above and then to work on it, would make it all worthwhile. I will let you know when it happens next in the NOI clinic.
David