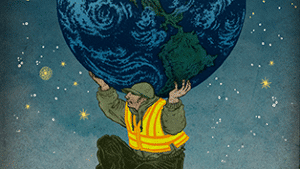
Illustration by Hanna Barczyk
Treating pain can be emotionally burdensome. Think about the last time a patient left the clinic and you lent back on your chair and let out a sign – it’s hard work. Each day that we respond to other people’s emotions we experience empathy.
“Once you open yourself to the suffering of others, it can feel impossible to turn off their pain.” (J. Zaki)
The stress of caring can lead to astonishing levels of job turnover. To avoid this, self-care is built into many professions where this is predicted – firefighting, paramedics, social work, psychologists, hospice care workers. Many other healthcare professions treat patients in pain but are traditionally thought to be more ‘manual’ or body focused. However, to tackle all the biopsychosocial elements of pain, these professionals need to have the resilience to be exposed to the plethora of emotions and stories shared by their patients as well. So how do you avoid empathy burnout?
“Medical students report lower levels of empathy as their training progresses. Health-care professionals underestimate patients’ suffering and even display blunted physiological signs of empathy for pain. Many helpers feel that they face a double bind. They can preserve themselves by growing emotional callouses and blunting their responses to those in need. Or they can throw themselves into building connections with their patients and risk being crushed by the weight of caring.”
An article in Nautilus by J. Zaki discusses another, perhaps more-favourable option, grounded in both neuroscience and psychology research. There is a distinction between two aspects of empathy that we are often not aware of:
Emotion contagion: vicariously sharing another person’s feelings – blurring boundaries between therapist and patient
Empathetic concern: forming a goal to alleviate a person’s suffering – strengthening boundaries between therapist and patient
Emotional contagion is often the driving factor that leads healthcare professionals into their career path. However, to foster sustainable, healthy empathy we are encouraged to practice the latter – empathetic concern. A key aspect of successful healthcare is the therapist’s ability to communicate warmth and understanding. Research indicates that emotion contagion impedes this, while empathetic concern facilitates it.
“Learning to practice one but not the other could be the best example of how caregivers can simultaneously look out for patients and for themselves. The distinction between contagion and concern does not come naturally. It takes conscious training.”
Luckily empathy, like many brain outputs, is not fixed. It can be adapted throughout the whole of life depending on the choices we make. Some suggest that we can practice compassion training to help avoid burnout – perhaps by fostering empathetic concern. Maybe it’s not so helpful to feel like we carry the weight of the world on our shoulders. Would it be more beneficial for all if, instead of putting ourselves in our patient’s shoes, we provide a face of resilience and compassion?
“Empathy is not one thing. Contagion and concern—two dimensions of empathy—need not travel together.”
– Hayley Leake
THE 2017 NOI CALENDAR IS SHAPING UP, HERE ARE THE CONFIRMED DATES
Melbourne 31 March – 2 April EP and GMI
Adelaide 26-28 May EP and GMI
Darwin 4 – 6 August EP and GMI
Brisbane 25 – 27 August EP and GMI
Newcastle 8-10 September EP and GMI
Details and dates coming soon for Wollongong and Sydney
Check out our courses page for details and to enquire
DAVID BUTLER IS HEADING TO THE UK AND EUROPE IN 2017
Eemnes, Netherlands – Explain Pain and Graded Motor Imagery April 22-24
York, England – Explain Pain April 26-27
Check out our courses page to make an enquiry
HAVE YOU DOWNLOADED OUR NEW PROTECTOMETER APP YET?

Just search the App Store from your iPad for ‘Protectometer’

I love the intent of this article – it is so important for those of us clinicians immersed in the work of helping alleviating the pain and suffering of others. However, I’m not sure the references back up the claims. The “compassion meditation” link takes me to a study that seems to show that practising this improves the clinical ability to identify the emotion of concern in the patient – nothing to do with protecting oneself from the cumulative burden of being immersed in others’ emotions. So good job for making this a focus – but I think we need some more concrete guidelines, all the better if they are research-based. If there are other leads you can give, I’d appreciate them.
Hey Alyssa,
Thanks for your comments and alerting me to this. You’re right, I’d linked the wrong study – since corrected. The correct link now takes you to a study titled ‘Differential pattern of functional brain plasticity after compassion and empathy training’ (Klimecki et al. 2014). The process of the training for empathy and compassion are included in their Supplementary Data file.
Kind regards,
Hayley
Hayley, one small point needs to be made here. We do not treat a “thing” called “pain”. Hopefully we treat fellow human beings who come to us hoping for pain relief.
Thank you for bringing empathy burnout to our attention. This is important for us to reflect on if we are to sustainably use ourselves with therapeutic intent to achieve optimal outcomes for our clients/patients. I have a closed group for health professionals (Thrive with Kimberley Kevan) where the sole purpose is for us, as health professionals, to consider and prioritise our own wellbeing and quality of life. I’ll be sharing this article on there. With gratitude, KK