![noinotes_march_2015large[2]](https://noigroup.com/wp-content/uploads/2020/11/noinotes_march_2015large2.jpg)
Ever since Explain Pain emerged in 2003, Lorimer Moseley and I have been asked by clinicians for a “simpler version… for patients”. We actually wrote something in 2005 but we resisted publishing this “short version” for a number of reasons – the data showed that people, even without medical training could get it – the material in “Explain Pain” wasn’t too hard or complicated, rather most clinicians underestimated their patient’s ability to learn about, and understand their pain. Additionally, and also important, the material was changing rapidly and so too were delivery modes. Remember YouTube only started in 2005.
Since Explain Pain, many clinicians have written their own short manuals – some are excellent, some are scary, others are plain wrong and many defy basic multimedia principles. We’ve noted that some, including published books and manuals, closely resemble the structure, text, ideas and style of Explain Pain, so much so that Lorimer and I can hear ourselves speaking when we read them!
Introducing The Explain Pain Handbook: Protectometer
The time seems right for the Explain Pain Handbook: Protectometer with its novel concepts of ‘DIMs’, ‘SIMs’ and the ‘Protectometer’. The Explain Pain Handbook: Protectometer is a short, interactive handbook for people experiencing pain. It was harder to write than any thesis or longer book than we’ve ever done, but hopefully we have it right.
Current thinking about pain allows this statement:
We will experience pain when our credible evidence of danger related to our body is greater than our credible evidence of safety related to our body. Equally we won’t have pain when our credible evidence of safety is greater than our credible evidence of danger (Moseley and Butler 2015, pp14).
There is such power in this simple statement. Lorimer is fond of saying that “it is as simple… and complicated as that”. There is a lot of danger ‘out there’ and it emerges from many domains. An example might be contained in an X-Ray report or what someone says or what you believe or hear on the news. There is a lot of safety out there too – such as accurate and up to date knowledge, having goals, help from a good health practitioner or being aware that someone loves you.
DIMs and SIMs
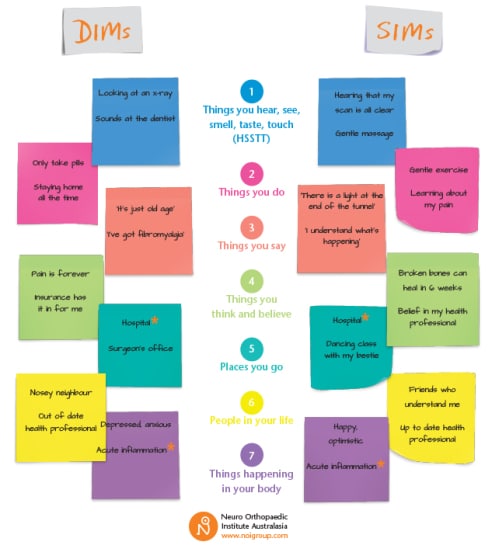
We call the dangers out there DIMs – Danger In Me, and the safety out there SIMs – Safety In Me. Each DIM or SIM must comprise distributed, context variable, neuroimmune circuitry in the brain – a unique ‘neurotag’ to use the language from Explain Pain.
We think that DIMs and SIMs can be organised into seven varieties…
Check out the examples above (and ponder some of your own). Note that there are things that are listed as both DIMs and SIMs? This is a reminder of the power of context. If your inflamed appendix has perforated, a hospital might be a very powerful SIM. If on the other hand, the hospital was where a previous surgery went wrong, the hospital might be one very big DIM. Similarly, a hot, red, swollen ankle an hour after ‘twisting’ is probably a DIM to most, but with the knowledge of the powerful self-healing properties of body tissues, the importance of inflammation and the likely timeframe to recovery, this DIM could become a SIM. Already there are signs pointing to potent interventions here, in particular, education.
DIMs, SIMs, The Protectometer and Pain
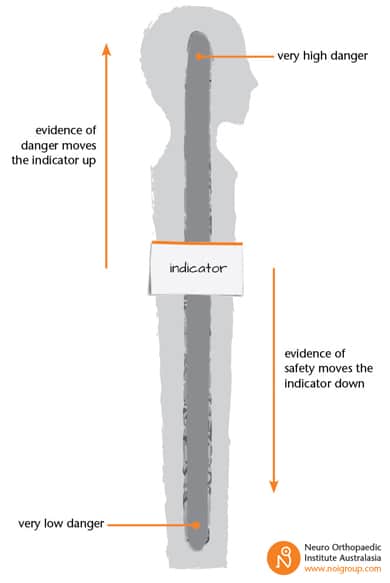
DIMs and SIMs are what ‘drive’ the Protectometer; the brand new pain education and treatment device in every Explain Pain Handbook – see the image below.
As credible for evidence for danger increases, i.e. DIMs increase in number or ‘power’, the indicator moves up. As credible for safety increases (more or more powerful SIMs) the indicator moves down. In the Handbook, we expand on the Protectometer a whole lot further – the top third of the Protectometer has the 0-10 pain scale that indicates that at a certain level of danger, an individual will start to construct a pain experience. The pain scale also demonstrates how increasing danger, adding DIMs from any category, can further increase pain, and we zoom in on the ‘alert zone’ – that area between ‘0’ and ‘1’ on the pain scale where even a small DIM might ‘tip’ someone into pain.
The power of the Protectometer
Using the Protectometer allows an individual (and their clinician) to map out all the many things – DIMs and SIMs – that collectively influence their pain experience. The therapy that flows on from this sounds simple – remove DIMs, and find and enhance SIMs. But “DIMs and SIMs can hide in hard to find places” – some deep self-reflection might be required. At the heart of the Protectometer is a subtle, but potent treatment effect – the possibility of a deep understanding and complete reconceptualisation of pain with potential for life long benefit.
The Protectometer is only half way through the Handbook – there is so much more packed in; a look at protective systems other than pain, such as the immune, motor, thinking and language systems. There is also the hope that bioplasticity brings, and treatment strategies that cover goal setting, moving smart, getting active, graded activity, unleashing happy hormones from the drug cabinet in the brain and cleaning up language. But they’re all for another noinote!
What is interesting is how quickly and easily the DIM SIM terms have caught on – I guess it is the food connotation perhaps hinting at the unknown ingredients within.
Thoughts, comments, questions, please, below.
David Butler and Tim Cocks

How do the dim and sim relate to migraine ?
Liesje, have you seen the movie ‘Cake’, with Jennifer Aniston?
Something she does near the end helps to relieve her pain. Her actions create a feeling of openness and connection and the pain eases. Have a look.
http://www.imdb.com/title/tt3442006/synopsis?ref_=ttpl_sa_2
Hi Liesje and Cam
The pain “formula” of “we will have pain when our brain’s credible evidence of danger outweighs credible evidence of safety” can apply to all pains..
Although most reasonable clinicians and researchers would agree that the pain experience is individual, unique and somewhat hidden from the world, a population view suggests there are also great commonalities – seen for example in biology (always peripheral & central processes) , in stigma, in response to treatment (often poor) , and in symptoms (eg “burning”, “pins and needles”).
However this commonality and its potential clinical use, is often adversely affected by geography (eg no one really wants to treat pelvic pain – knees are far more “acceptable”) and diagnosis (eg chronic low back pain, diabetic neuropathy and multiple sclerosis share many symptoms including pain and paraesthesia and thus treatments should be similar).
I suggest that treatments based on a symptom and pain experience profile, to some degree regardless of geography and diagnosis may enhance inclusion of pain problems that are missed or where people wonder “does my pain fit into this treatment”.
So “yes” – the DIMs, SIMs and Protectometer concepts will fit headache, including migraine. As we suggest in the Handbook, every condition should get ‘checked out’ medically with, ideally, any investigations interpreted and explained by a clever clinician with a good understanding of modern pain biology. If there is nothing requiring medical management, which is usually the case, treatment would proceed in line with finding and removing DIMs and addings SIMs. Knowledge would seem to be the key here. DIMs will likely be present in all seven categories including things happening in your body, things you do, even the places you go and the people you meet. Considered self-reflection will be valuable here. In the handbook, we also talk about acknowledging and accepting that perhaps some DIMs can’t be changed, but understanding the Protectometer allows hope that those DIMs that can be removed are, and that SIMs can always be found.
Many successful pain treatments have been using similar notions already.
Best wishes
David
In fact most movies have a point where the protagonist faces an obstacle he needs to overcome. His difficulties build exponentially until he is forced to change his perspective or adopt a new behaviour in order to break through – aka, a SIM.
‘Groundhog Day’ is a perfect example of ‘SIM stacking’. The lead character finds himself well and truly stuck in every way imaginable. He finds a solution when he begins to identify SIMs and then stack them end on end, moving rapidly from one to the next. The momentum he creates is very obvious and the boost he feels allows him to identify and release some DIMs. He also changes quite a few DIMs into SIMs. As mentioned above, many of these DIM/SIMs are unrealized because they are buried quite deeply. And it ends well – he gets the lead female into bed!
I know I harped on about the addiction thing in a previous post, but ‘Groundhog Day’ handles this quite well. The lead’s changes create a ‘flow’ where he naturally moves from one SIM to the next, instead of getting stuck again. But I can’t help thinking: How would a writer construct a follow up to that movie? What happens next? Does Bill Murray live in perfect happiness ever after? Many philosophers would say he would go full circle and eventually seek misery and difficulty once again, even if this was a subconscious process. I’m not sure I like thist idea, but I can see the truth in it. Man’s premier addiction is to drama and ‘problem solving’. We simply cannot get enough. Do we create all these obstacles in order to enjoy the process of overcoming them? What if problems were reconceptualized as “just what is”?
Anyway, back to fixing my own life. Another plate of dim sims with extra soy sauce! 🙂
Regards, EG
As I commented on Pelvic Pain I totally agree David that the geography is irrelevant if we address that which the patient is presenting with.
EG, we all have our Dims & Sims but equally we all have the capacity to stack them in our favour if we so choose. It is our consciousness, we own it and we can do with it as we please, if we are prepared to take responsibility for it…….
DB
London 😊😊😊
I have a patient at the moment who wants so much to buy into the “Pain story” but struggles to fully embody it. I feel that the Dim holding her back to be psychological wounding from the past deeply buried in her subconscious. Proof of this has surfaced just recently, when I finally encouraged her to see our psychotherapist. She basically lost it during a session and wanted to run away. The discussion was getting to ” Close to the bone” for comfort. Without the Protectometer hand book I was struggling to get through to her. I had run out of ideas. We are now working with her Dims & Sims and she is beginning to see that the events during the psychotherapy session do confirm my direction with her.
Some of my language may sound strange coming from a physiotherapist but we don’t have to be a psychotherapist or well read in philosophy to practice Biopsychosocial medicine. We just need to have courage to face the unexpected that might emerge from the patient and remain human and compassionate. The rest is practice. To quote Lorimer ” it’s that simple and that complicated”
Thank you guys for yet another supurb tool for the toolkit. Job well done and maybe another patient will begin to shift her Dims to Sims.
Hugs and champagne all round
DB
London👏👏👏😎
Couldn’t agree more with the concept. As a practicing physiotherapist and a moderate mileage runner i am able to sustain my running loads in the presence of same injuries i have to at times ask my patients to rest a week or so , simply cos i am easily able to undermine the DIMs and treat them as SIM’s out of my sheer knowledge that comes with being a therapist.
Geography hardly plays a role cos the ‘ pain experience’ as i like to call it is so so unique yet is so easily classified in multiple spectrums in my existing patient population ( 15 years of first contact practice in my populous nation India) . Be it the neck , the low back or a chronic ankle , or headaches i am sure the DIM TO SIM journey though needs hand holding is surely going to be a ride !
DB,
I reckon the words “how about seeing a psychologist?” represents a massive DIM for most chronic pain clients. It triggers all sorts of deep fears, and in that sense can worsen symptoms. That’s why I don’t recommend psychologists, even though they could be very helpful. My clients don’t know I’m working on their mind. It’s all done under the guise of physio. I might be rubbing their shoulder but as I’m talking I’m using metaphors, covert suggestions and all sorts of tricky hypnotic patterns. And they work AMAZINGLY well.
Anyone who ‘loses it’ during a consult has been confronted with material the ego is not ready to face. If the psychologist has triggered that, then that’s unskillful practice. It’s difficult to progress when this has happened because instead of feeling safe, the client now feels threatened. Ego defenses absolutely MUST be respected. And since most chronic pain clients have very strong ego defenses (protecting a fragile self-image), the direct approach will not work. Smoke and mirrors is the way to go.
Regards, EG
I agree
Having said that, I currently have two clients reading Protectometer. My preference would be for chronic clients go straight to educational material such as this and fix themselves, but this is not often practical for the reasons mentioned. The material itself can be perceived as a DIM.
EG.
EG ,
It is just the same at my end of practice too. Conversations form the most integral component of therapy as integral as the manual therapy . The relationship that bulids over time makes it a lot easier to slip in concepts entirely radical to pre existing mindsets yet imperative to convert dims into sims.
Regards, CC
A psychotherapist trains for a minimum of seven years to achieve their qualification and privilege to work with the human consciousness through the unconcious mind.
Modalities, such as cognitive behavioural therapy, neurolinguistic programming and hypnotism are just that, modalities which should only be used by qualified people.
People outside the psychotherapeutic professions using such modalities very quickly title themselves a “Therapist” and that’s where the “Real” danger begins for the patient.
We have the same problems in our profession with people, of little skill, calling themselves Therapists and Experts of that modality with no knowledge to ask and answer the Golden Questions:- what’s wrong, what has to change, how can change be brought about together, how long and how much will it cost.
If we are going to help our patients, we sometimes need help from other disciplines such as social workers, psychotherapists etc. If that means, initially raising their anxiety and creating a short term DIM, in a ” Safe environment”, then I believe that to be for the long term good of the patient. Because I’ve asked and answered some of my Golden questions, through the core of my skill” Clinical Reasoning” my patient is held in that said, Safe Environment.
The real danger to the patient and the risk of a “Reaction” comes from practitioners applying teqniques when they don’t have the professional training-clinical reasoning capacity- to administer them and , more importantly handle the outcomes both positive and negative. To take the credit for a good outcome is easy. To take the credit for a poor outcome more challenging and will show the real steel of the practitioner.
By the way, even a highly skilled psychotherapist with forty five years of clinical experience can’t see everything that might emerge from a client. Indeed I still get it wrong sometimes myself and, in good old fashioned Maitland style have got my “SIN” wrong………
DB
London😇😇😇
DB, see how when I challenge you it creates problems? See how progress is now stifled between us? My challenges were legitimate, but see how you’re a bit miffed with me now? It’s fair enough, I feel a bit miffed with you too. Why is that? It’s because I was blunt – I triggered your ego defenses and now you are trying to trigger mine.
THAT WAS MY POINT! – not to do that with clients because it shuts down progress. I am not subtle in here because I’m dealing with other health professionals and we desperately need to GET REAL. Not having the courage to be real is what is holding the profession back. Clients are a different kettle of fish – they need to be handled with much greater subtlety.
Education is so freely available online nowadays. Anyone who wants to become an expert can do that using Google, Amazon and forums such as this. You just keep clicking away for 10 thousand hours, and reading and reading and reading….
When you find someone who is advanced, contact him and pick his brains. I did this many years ago when I first came across Dave’s work. And I have done it with countless others – hypnotists, psychologists, neuroscientists, philosophers.
A piece of paper with a qualification means very little to me nowadays. I learned virtually nothing useful in my 4 year Physio degree. It was a horrible waste of time and money and effort. To say that I don’t recommend psychologists to clients is in no way an attack on psychologists. As Physios we have a great advantage in that we can utilize psychological principles without the client knowing – all for his great benefit. Aside from that, I can run rings around most psychologists, hence my confidence. When I detect a hole in my knowledge base, I hit Google hard and patch it up. I certainly don’t go back to university.
EG.
PS. In your first post you said: “…We don’t have to be a psychotherapist or well read in philosophy to practice Biopsychosocial medicine”.
versus…
This: “The real danger to the patient … comes from practitioners applying teqniques when they don’t have the professional training-clinical reasoning capacity- to administer”.
I love DIM SUM… opps its DIM SIM. Love the ingredients in it too! 🙂
I just used this with my current pain rehab group, who I can hear chatting and laughing over morning tea in the next room…
It went over very well, with real meaningful examples which stimulated further discussion about their own DIMs and SIMs
A very nice, digestible analogy…
A patient breezed into my practice today, as I happened to be sitting at the front desk and asked ” What is that smell, I’ve noticed it each time I come in here, it reminds me of something “? I immediately, yet discretely checked my armpits and breath feeling very exposed and somewhat panicked. I enquired, what smell might that be, and felt reassured as a pleasing yet searching smile spread across her face. I made a few suggestions as to its nature, each of which was met with no, no not that then, illumination filled her eyes as she replied “It smells of safety”. Wow what a beautiful SIM I thought……..
DB
London 😱😱😱😀😀😀
EP3 was worthwhile, thanks all.
I can’t fathom how this material is not part of the undergraduate course work for physios. Where are we on that front?
I have been dabbling with the concept of DIMS and SIMS and quite successfully so. All of my patients have responded with “that makes a lot of sense” and then we work together through the sessions (through their laughter or tears) about any comments that could be a DIM or a SIM. It is so wonderful when I see the the light bulb light up and get their wheels turning toward making a connection to their pain. I turn it into a verbal game with the patient by keeping a rough score (dims vs sims) through our discussion of discovery/ assessment. The terms roll off the tongue easily. As a clinician, I find it light enough to be non-threatening way to discuss life’s stresses and joys and how that might contribute to their pain experience by modulating the processing of the nervous, immune, and endocrine systems. Thank you for your work on the Protectometer!
Thanks Kara(?) We love to hear from clinicians out at the coal face exploring the new world of DIMs and SIMs.
Using a Protectometer, as found in The Explain Pain Handbook: Protectometer might make the game visual and tactile as well as verbal and make it easier to keep track…. 😉
Jokes aside, your point about DIMs and SIMs being a gentle way in to discussing a range of issues is so important – for some people, even a caring clinician asking what are perceived to be ‘probing’ questions might be another DIM.
Thanks for sharing
My best
Tim
Reblogged this on karenpriceblog and commented:
Another Reblog. Sourced from another clinician colleague on GPSDownUnder closed Facebook group for Australian and New Zealand GP’s.
I thought this was a great article explains the complexity of the pain experience to both clinicians and patients.
The DIM -SIM model may well help our consultations with these very complex patients
By deconstructing and reconstructing the pain there may well be advances in recovery and therapeutic relationship.
This looks like a great tool and has been recommended to me by my medical team, but is limited to those with iPads? Is there any possibility of it being available on Android please? Thank you.
Hi,
The Protectometer App is exclusive to iPad at the moment, and we don’t have any plans to develop a version for Android – there are a range of technical issues that make an Android version difficult to do for this App.
However, the book version – The Explain Pain Handbook: Protectometer is available for everyone – http://www.noigroup.com/en/Product/EPHPB
Best
Tim
Thanks for the response Tim
There is no question that unhelpful language keeps me in a job. Right up there with medical letters that people don’t understand. However, there is also what the patient infers from what has been said. So no matter how well I think I’ve explained something, people in pain have to somehow discard everything they’ve been told in the past, which is a big ask. I like the idea of alliteration.
As a psychologist working with many trauma clients, I use the Protectometer DIMS and SIMs to both explain what is happening for them and how to move towards recovery. If you re-read this post and replace PTSD where it says pain… well, it just works 😀
Hi Terri, great to hear that as I often work closely with psychologists and psychotherapists and the protectometer is equally a wonderful tool to show patients that there is more to their pain than the body part. This provides the hook to suggest “talk therapies” will help and gets them to try in situations where they would otherwise never have considered it…
DB London 😎
Are you saying that once a patient no longer fears pain, or whatever ‘Dims’ they have, then their pain will be gone?
This worksheet is incredibly useful. I started using this more often in my clinic and the feedback I receive from my patients are awesome! Thank you for making it available for printing online.
Greetings,
Erkan Onurlu, DDS, DABOP