After writing two of the most popular posts on noijam in 2017, Professor Sonia Grover is back again to share her expertise and knowledge. In this post, Professor Grover takes you deeper into some of the biology involved in period pain.
From strict definitions to practical perspectives
I’m sure I can hear someone saying, ‘When will she start talking about ENDOMETRIOSIS – surely that is the most important cause of period pain?’ and ‘What about all the other things that contribute, like central sensitisation??’
Well, I’m getting there, but I would like to talk about how heavy periods and retrograde bleeding are related to period pain first.
Let’s start with defining heavy periods. Although there are ‘strict definitions’, from a practical perspective changing pads or tampons more often than every 2 hours (because if you didn’t you would have a disastrous mess), or needing to put a towel under you at night in bed, or getting up overnight to change pads, are all things that tell me as a gynaecologist, ‘yes- ok, that is a heavy period’.
Sometimes women report that they are passing clots. In general we don’t actually worry about clots – it simply tells us that your bleeding/clotting system is working and that the time taken for the blood to leave the blood vessels in the uterus and get to the outside world has been long enough for it to clot (which is good news!) But big clots, (that is clots bigger than 50cent pieces or clots that fill the palm of your hand), they tell us you are bleeding heavily.
So, if your uterus is trying to expel, squeeze out a big clot – it might need to squeeze extra hard and that can make extra pain! So making periods lighter (or skipping periods) can reduce or stop this extra crampy pain.
Backward flowing periods or “retrograde bleeding”
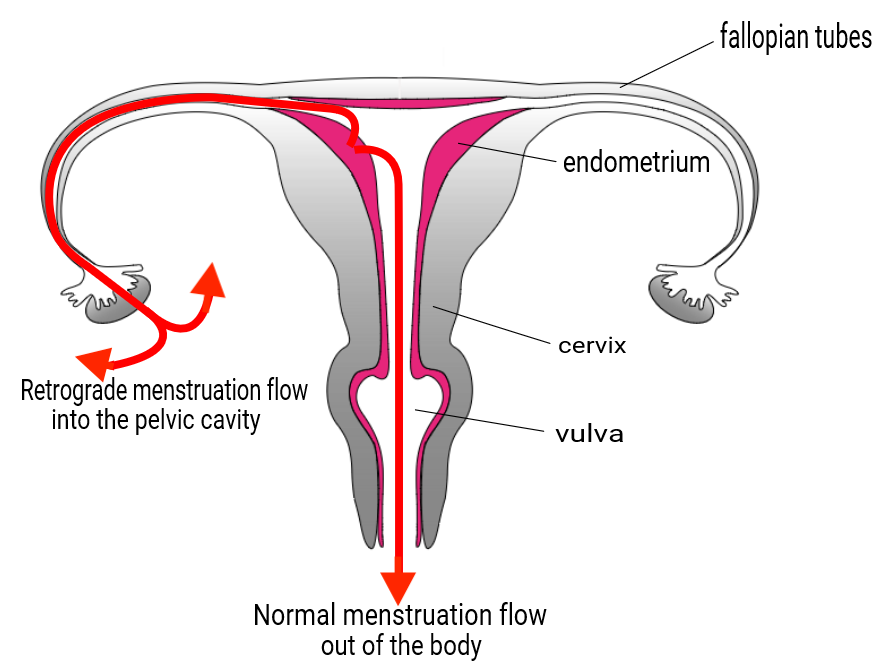
Women who have heavy periods are more likely to have more retrograde bleeding, that is, period blood flowing backwards. Some backward flow actually happens in just about all women, but there are a few things that can make this worse.
It occurs more in women who have heavier periods. It also occurs when there is some sort of blockage or narrowing so that the blood can’t easily come out of the cervix or through the vagina. Then there are some things that probably have an impact but have not been so well studied. These include consideration of the actual dimensions of the 3 openings from the uterus- the 2 tube openings and the cervix – which we know vary in their shape and size, as well as the strength and direction of the uterine muscle contraction.
The back flowing of period blood does several things
The blood itself sloshing around on your insides can be painful. We know your body will reabsorb this – just as it reabsorbs bruises and swelling – but the blood can irritate the surfaces on the inside, including the bladder and bowel surfaces. I usually try to describe this by reminding people what it feels like to get sunburnt – inflamed, irritated – shoulders. (I know we are not supposed to get sunburnt, but at some point most of us have…) Well if your shoulders are sunburnt – it hurts to touch or move them, but it is usually ok if you sit there still, not moving. So, when you have blood sloshing around on your insides, you want to lie still and it hurts to empty your bladder and use your bowels, as the surfaces of the bladder and bowel are ‘sunburnt’ and irritated. This can be highly uncomfortable, but it passes, and for many women understanding the biology underlying this process can help reduce the worry, and some of the pain.
There are a number of approaches that I can recommend to women experiencing pain associated with heavy periods and retrograde bleeding. First is to reduce bleeding by using a specific non-hormonal medication called tranexamic acid- you will need a prescription from your doctor for this. Second is making periods lighter or actually skipping them by using the oral contraceptive pill, or other hormonal medications. A hormonal intrauterine system will also help avoid both of these types of pain.
The elephant in the room
I will mention the word endometriosis at this point – as the main theory regarding the development of endometriosis relates to retrograde menstrual flow. The retrograde bleeding carries with it more than just blood. There are a multitude of potent chemicals (remember the pro-inflammatory cytokines and inflammasomes from my first blog) and cells – including endometrial cells from the lining of the womb (I mentioned that you could see these under a microscope if you wanted to, in my first blog). The idea is that retrograde menstrual bleeding is probably how the endometrial cells end up on the outside of the uterus and fallopian tubes in the first place.
We know that women who have heavy periods are more likely to have endometriosis and we also know that women who have lighter periods are less likely to have endometriosis. And I can also tell you that women who have no uterus (about 1 in 4000 women are born without a uterus) do NOT get endometriosis. Clearly there is a link, but we don’t fully understand it yet.
So having lighter periods, or avoiding periods not only will help reduce or avoid period pain, but will also reduce the likelihood of developing endometriosis.
Still telling the truth
In my first blog, I wrote about the truth of having a period – emphasizing both the completely normal and natural process that periods represent, along with the amazing biological complexity, and the significant changes that take place. For many women, heavy bleeding and retrograde flow is normal, but they can add even further to the complexity and for some women contribute to period pain. Additionally, the links between heavy bleeding, retrograde flow and endometriosis suggests that the combination of these might lead to a situation that is not normal.
The good news is, we understand this process reasonably well, can explain it to women to reduce fear and worry, and medically intervene where appropriate, to reduce or even eliminate pain.
-Sonia Grover
 Professor Sonia Grover has extensive experience in paediatric and adolescent gynaecology having worked in this field for over 20 years. She has been instrumental in establishing this subspecialty in Australia as well as in Asia and internationally. Professor Grover’s clinical interests include all aspects of young women’s’ reproductive health – including menstrual problems (excessive bleeding and/or pain), amenorrhoea, ovarian problems, congenital anomalies affecting the reproductive tract and reproductive hormones and the cyclic exacerbation of ‘non-gynaecological symptoms’ including cyclic seizures, asthma, and chronic fatigue. Professor Grover’s ResearchGate profile here.
Professor Sonia Grover has extensive experience in paediatric and adolescent gynaecology having worked in this field for over 20 years. She has been instrumental in establishing this subspecialty in Australia as well as in Asia and internationally. Professor Grover’s clinical interests include all aspects of young women’s’ reproductive health – including menstrual problems (excessive bleeding and/or pain), amenorrhoea, ovarian problems, congenital anomalies affecting the reproductive tract and reproductive hormones and the cyclic exacerbation of ‘non-gynaecological symptoms’ including cyclic seizures, asthma, and chronic fatigue. Professor Grover’s ResearchGate profile here.

These period posts have been unbelievably helpful in understanding my own body as well as being better able to explain the impact of periods for my patients in pain. Thank you so much for writing!
Thanks for this interesting article. Is this potentially a reason to avoid spending time in upside positions? (For example, athletes such as gymnasts.)