Editor’s note: NOI US Instructor Ben Boyd, and his colleagues Marc Broberg and Tamara Backer have recently published a reflection on delivering pain education. Using a single case study as an example, Ben, Marc and Tamara offer novel insights from multiple perspectives and provide deep reflections from their point of view as clinicians delivering education in an interprofessional setting. We think the paper offers extremely valuable insight, so we invited Ben and Marc to share the paper with our audience and write a post to explain how it came about and where their experience sits within the current literature on Explaining Pain. We’ve added a few snippets from the paper to give you a taste and hopefully whet your whistle! Our sincere thanks to Ben and Marc for sharing the following.
How to Explain Pain?
While the science, narratives and stories behind the pain science revolution are fascinating, relevant, and important to many patients and clients, we often hear…
- How do I do it?
- Where do I start?
- What does this specific person in front of me need to know?
- I tried that once and it didn’t go well… not doing that again
- How do I integrate this patient education into the other aspects of care, such as exercise, movement-based therapies, manual therapy, etc?
- That all sounds good but how do I apply that to complex, real-world situations?
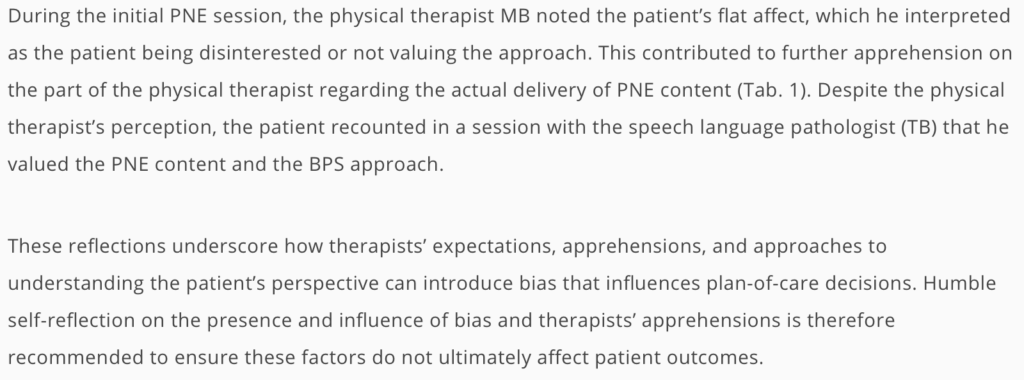
Questions similar to these led to our collaboration on a complex patient case. The situation was complex in many ways; including a traumatic event associated with the start of the patient’s pain, a history of drug abuse, severe pain and disability, and the challenges of multiple healthcare practitioners delivering care. In addition, there was a wide variance in understanding of, and skill in delivering education about modern pain neuroscience.
One of us (MB), is an experienced physical therapist who had read lots about pain neuroscience but was novice to delivering it clinically. The other (BB), teaches about pain in entry-level and post professional settings regularly but is not consistently in the clinic. The following case report is the result of this collaboration.
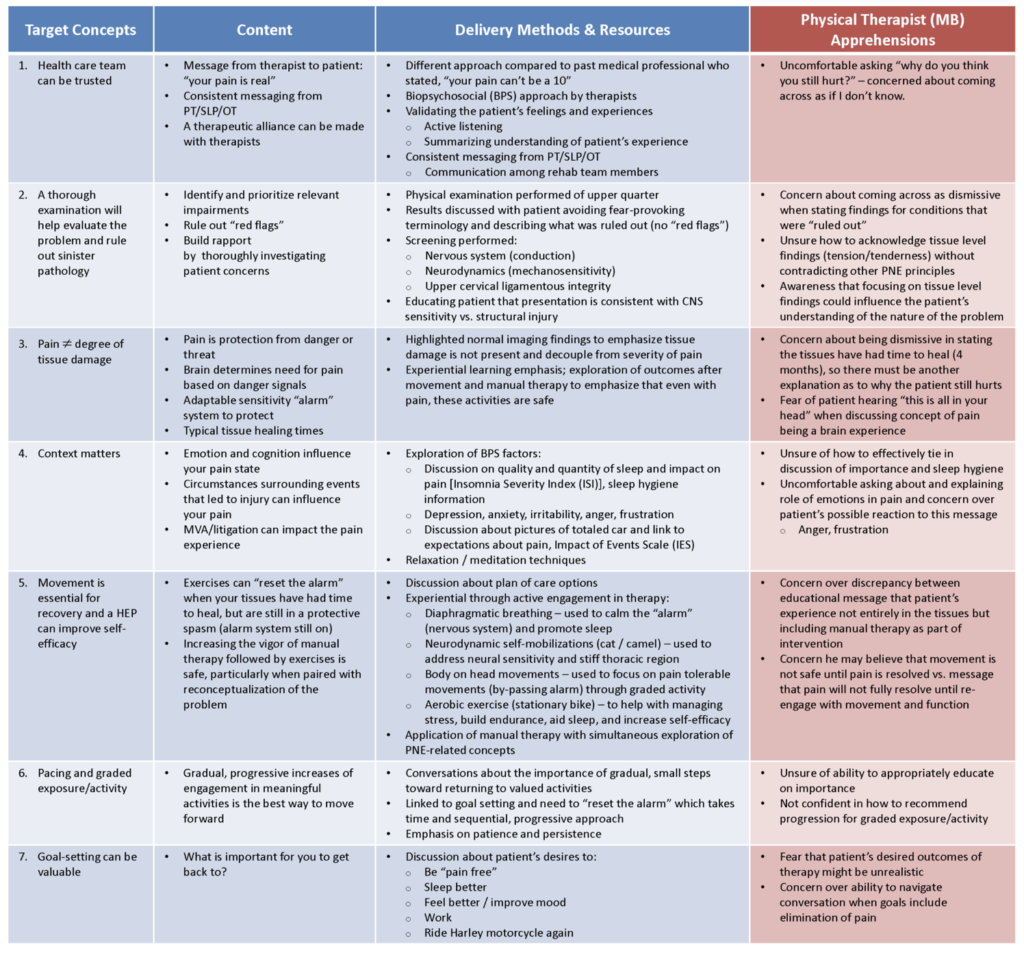
We explore several themes that highlight the challenges of “Explaining Pain” in this real world case example. We discuss the development of the components of a pain neuroscience education (PNE) curriculum (target concepts, content, delivery method and resources) designed specifically for the circumstances of an individual patient suffering from severe pain and disability. We evaluate the apprehensions of a therapist novice to delivering PNE, including both successes and barriers. We look at the impact drug addiction had on the outcome of this case. We explore the self-reflections of the patient and members of the rehabilitation team. Lastly, we look at the challenges of interprofessional teamwork in an outpatient setting.
Comparison to the literature
A recent mixed methods systematic review (Watson et al 2019) highlighted that PNE can help people cope better with their condition, reduce fear about movement related to their pain, and reduce catastrophizing. However, they did not find that PNE changes pain or disability over time. Importantly, they highlight the value of the patient feeling heard and the importance of the patient reconceptualizing their pain.
Similar to their findings, the patient in our case report did demonstrate behaviors consistent with less fear and was more engaged in his life at the end of his care. He also reported feeling heard for the first time and appreciated delving into the emotional aspects of his situation in addition to the physical dimensions of his injury.
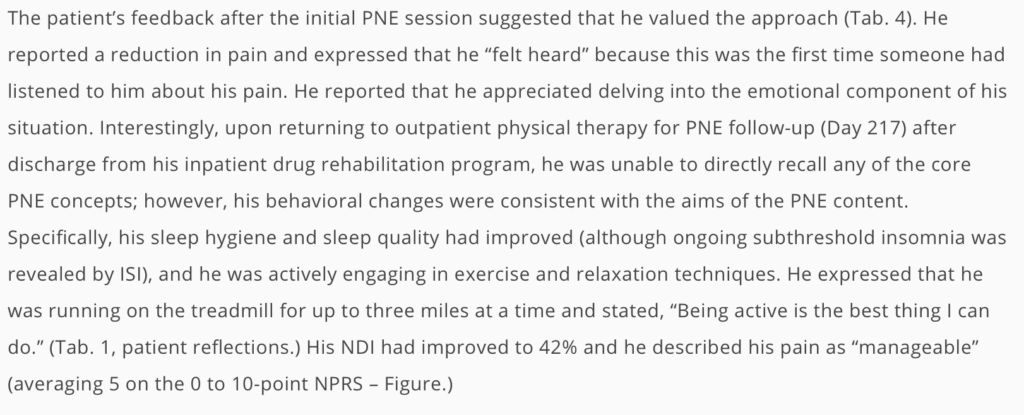
It is interesting to note that the patient described in our case report did have significant reductions in his pain and disability, which is in contrast to the findings of Watson et al’s (2019) systematic review. Their review represents the pooled outcome of multiple research studies from various countries where various designs of PNE were delivered to a wide variety of patient groups suffering with chronic musculoskeletal pain. Some of this variety includes PNE delivered in a rehabilitation setting or in an educational institution; via face-to-face groups, through written materials, or a combination of methods; delivered in one session or over multiple sessions; with a total time for delivery ranging from 30 minutes to 3 hours.
We feel there is value in both large-scale systematic reviews that explore the overall group findings of a priori PNE programs as well as individualized, patient specific PNE delivery as is presented in case reports such as ours. The latter provides a real world example of attempts to develop and deliver patient centered PNE within a complex patient scenario. We hope that people can use this care report as a tool to help guide their own explorations and reflections as a means of answering some of the questions about how to explain pain posed above.
We hope you find value in this work!
All the best,
– Ben Boyd and Marc Broberg
 Ben Boyd (PT, DPTSc, OCS) is an Associate Professor at Samuel Merritt University in Oakland, California, where he primarily teaches in the Doctor of Physical Therapy Program. Additionally, Ben has been teaching pain education and treatment content to health care practitioners for the Neuro Orthopaedic Institute (NOI) since 2013. He has worked as an outpatient Physical Therapist in multiple orthopedics, hospital-based, and private practice settings. Ben’s research emphasis is neuropathic pain, specifically focusing on the evaluation and treatment of mechanosensitivity of the nervous system associated with Diabetes Mellitus breast cancer treatments. Ben has a passion for understanding the complex and personal nature of pain experiences with the hope of helping alleviating suffering.
Ben Boyd (PT, DPTSc, OCS) is an Associate Professor at Samuel Merritt University in Oakland, California, where he primarily teaches in the Doctor of Physical Therapy Program. Additionally, Ben has been teaching pain education and treatment content to health care practitioners for the Neuro Orthopaedic Institute (NOI) since 2013. He has worked as an outpatient Physical Therapist in multiple orthopedics, hospital-based, and private practice settings. Ben’s research emphasis is neuropathic pain, specifically focusing on the evaluation and treatment of mechanosensitivity of the nervous system associated with Diabetes Mellitus breast cancer treatments. Ben has a passion for understanding the complex and personal nature of pain experiences with the hope of helping alleviating suffering.
 Marc Broberg, PT, MSPT, NCS is part owner of Two Trees Therapy and Wellness in Ventura, CA. He works primarily with individuals recovering from brain injury and vertigo. Marc is interested in enhancing the therapeutic alliance through the exploration of biopsychosocial influences on the rehabilitative experience. Marc wrote this paper from a vulnerable perspective to reveal the internal challenges.
Marc Broberg, PT, MSPT, NCS is part owner of Two Trees Therapy and Wellness in Ventura, CA. He works primarily with individuals recovering from brain injury and vertigo. Marc is interested in enhancing the therapeutic alliance through the exploration of biopsychosocial influences on the rehabilitative experience. Marc wrote this paper from a vulnerable perspective to reveal the internal challenges.
Related ‘jams
After the Lancet papers on back pain, get your explain pain game on
Building a simple curriculum
Relevant reading
Bodily Relearning, Boyd BS
Explain Pain Second Edition, Butler & Moseley

I was surprised to learn that modern pain neuroscience is teaching clinicians that “pain is protection from danger or threat” and that “the brain determines the need for pain based on danger signals.” The first quote depicts pain as a “thing” with agentive properties, when we all know it is simply a word we use to describe a particular experience. The second quote incorrectly (in my view) attributes decision-making to the brain when such a function is performed by the person.
The other point I would like to make is that Professor Lorimer Moseley now concedes that humans experience pain, which negates “the concept of pain being a brain experience” – as appears in your Table under the heading “Physical Therapist (MB) Apprehensions”
Can I get a copy of this? It didn’t work when I clicked on it. Targeted curriculum developed for the specific case (click for full sized image).
Hi Kristin, the paper is freely available (with all content) at any of the links.
Cheers
Tim